Document
advertisement
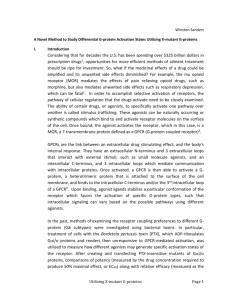
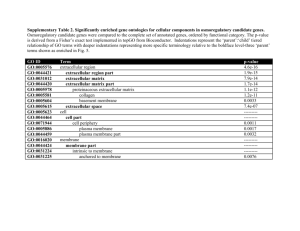
Advanced Bioinformatics Lecture 6: Pharmacology and drug development ZHU FENG zhufeng@cqu.edu.cn http://idrb.cqu.edu.cn/ Innovative Drug Research Centre in CQU 创新药物研究与生物信息学实验室 Table of Content 1. Modern drug development 2. Drug & corresponding target 3. Mechanism of drug binding 4. Mechanism of drug action 5. Adrenoceptor cardiac function 2 2013 ranking of the global top 10 pharmaceutical companies based on revenue 40.0 + 15.0 + 3.8 + 1.8 = 60.6 Revenue in billion U.S. dollars 3 Top 10 drugs ranked by sales for Q1 2013 Rank Brand Name(s) Generic Name Sales (billion USD) Company Therapeutic Class Approval Year 1 Abilify Aripiprazole 1.5 Otsuka, BMS Depression 2002 2 Nexium Esomeprazole 1.4 AstraZeneca Dyspepsia 2000 3 Cymbalta Duloxetine 1.3 Depression 2004 4 Crestor Rosuvastatin 1.3 Eli Lilly AstraZeneca, Shionogi Cholesterol 2002 5 Seretide Fluticasone + Salmeterol 1.3 GSK Asthma 2000 6 Humira Adalimumab 1.2 Abbott Rheumatoid arthritis 2002 7 Enbrel Etanercept 1.1 Amgen Rheumatoid arthritis 1998 8 Remicade Infliximab 1.0 Rheumatoid arthritis 1998 9 Copaxone Glatiramer 0.9 J&J, Merck Teva, SanofiAventis Multiple sclerosis 1996 10 Neulasta Filgrastim 0.9 Amgen Neutropenia 2002 4 Traditional drug design Random screening against disease assays Natural products, synthetic chemicals, etc Long design cycle: 7-12 years High cost: 350 million USD per marketed drug Too slow and costly to meet demand Drug Discovery Today 2, 72-78 (1997) 5 Modern drug development Rational drug design and testing Speed-up screening process Efficient screening (focused, target directed) Computer aided drug design (target directed) Integration of testing into design process Fail drugs fast (remove hopeless ones AEAP) 6 Strategies for improving design cycle Smart screening: − High-throughput robotic screening Diversity of chemical compounds: − Combinatorial chemistry High expectation Nature 384 Suppl., 2-7 (1996) 7 Any other alternative approach? Current situation: − Molecular mechanism of disease processes, structural biology. − Rising cost of experimental equipment and resources. − Computer revolution (low cost, high power). − Software development. Natural conclusion: computer approach? 8 Strategies for improving design cycle Computer-aided drug design: − Receptor 3D structure unknown Receptor-based drug design (QSAR) − Receptor 3D structure known Ligand-based drug design (Docking) Science 257, 1078-1082 (1992) 9 The stages of development of a ‘typical’ new drug Overall cost per marketed compound is ₤250-500 million and the typical time scale is 8-12 years. Only about 1 in 12 entering development succeeds in reaching the market 10 Key go/no-go decisions for developing a drug Key decision gates in drug development Drug candidate selection Key questions and pivotal studies Bio-stability Metabolism Bioavailability Cytotoxicity Dosage Synthesis Formulation 12 Drug safety indicators Key questions and pivotal studies Formulation Dosage Safety margin Metabolism Metabolism Effects on heart Effects on lung 13 Pharmacology today with its various subdivisions 14 Drug & corresponding target 15 Drug target: receptor Receptors are the sites at which molecules such as hormones and neurotransmitters are recognised. A drug that binds to a receptor can be: Agonist: trigger the same events as the native ligand. Antagonist: stop bind of the native agent without eliciting a response There are four ‘superfamilies’ of receptors 16 Types of receptor-effector linkage 17 Drug target: enzyme Proteins catalyzing reactions required for cellular function. Specific for particular substrate or family of substrates. Inhibitor restricts action of enzyme on its substrate. Inhibitors may be irreversible or reversible. Reversible inhibitors: Competitive & Non-competitive. Enzyme inhibitors might be seen to allow very ‘fine control’ of cellular processes. 18 Drug target: nucleic acids Designing compounds that can distinguish target nucleic acid sequences is not yet achievable. There are compounds with planar aromatic regions that bind in-between the base pairs of DNA or to the DNA grooves. These generally inhibit the processes of DNA manipulation required for protein synthesis and cell division. Suitable for aiming at promoting cell death. 19 Bio-chemical class distribution for successful & clinical trial targets Fig 1 BioChemical Class Distribution for Successful Targets (348) Channels and Transporters 12% Receptor 24% Factors and Regulators 6% Nuclear Receptor 4% Binding protein/Antigen 4% Enzyme 46% Structure Proteins 3% Nucleic Acid 1% Fig 2 BioChemical Class Distribution for Clinical Trial Targets (295) Receptor 24% Channels and Transporters Factors and 8% Regulators Nuclear Receptor 11% 1% Binding protein/Antigen 5% Structure Proteins 3% Enzyme 40% Nucleic Acid 8% 20 Mechanisms and specificity of drug binding The majority of binding and recognition occurs through noncovalent interactions. These govern: The folding of proteins and DNA. The association of membranes. Molecular recognition (e.g. interaction between an enzyme and its substrate or the binding of an antibody). They are generally weak and operate only over short distances. As a result large numbers of these interactions are necessary for stability, requiring a high degree of complementarity between binding groups and molecules. 21 Drug binding site in a cavity of protein HIV-1 protease 22 Mechanism of drug binding and actions Lock and key: blocking => stopping of protein function HIV-1 protease complex with SB203238 23 Covalent bonds The ‘sharing’ of a pair of electrons between two atoms. A very stable interaction Requires hundreds of kilojoules (kJ) to disrupt Compounds that inhibit enzymes through formation of covalent interactions are called ‘suicide inhibitors’. Not all covalent bond formation is irreversible Hydrolysis Action of repairing proteins 24 Non-covalent interactions The forces involved are: Hydrogen bonds van der Waals forces Ionic / electrostatic interactions Hydrophobic interactions Generally, such interactions are weak: Vary from 4-30 kJ/mol 25 Selectivity, toxicity and therapeutic index Drugs may bind to both their desired target and to other molecules in an organism. If interactions with other targets are negligible then a drug is said to be specific. In most cases drugs will show a non-exclusive preference for their target - selective. The interaction with both their intended target and other molecules can lead to undesirable effects (side effects). 26 Selectivity, toxicity and therapeutic index Establish the concentrations at which the drug exerts its beneficial effect and where the level of side effects becomes unacceptable. Commonly used values are ED50 and LD50. For obvious reasons LD50 tests are not carried out on human volunteers! One measure of the margin of safety is the therapeutic index. Therapeutic index = LD50 / ED50 Drugs with low therapeutic indices are only used in ‘life or death’ type situations. 27 Agonists & antagonists Activity of a drug is the result of two independent factors: Affinity is the ability of a drug to bind to its receptor Efficacy is the ability of the bound drug to elicit a response There are 2 classes of agonist Full agonists – which elicit the maximum possible response at some concentration Partial agonists – which never elicit the maximum possible response from the receptor There are 2 classes of antagonist Competitive – which compete for the agonist binding site, and require higher agonist concentration to elicit a given response. Non-competitive – these bind at a site other than the agonist binding site, or even to a completely different molecular target. The result is the lowering of the maximum possible response in addition to the usual antagonist effect of ‘displacing’ agonist activity to higher concentration. 28 Case study Adrenoceptor and control of cardiac function Adrenoceptor is receptor for two important hormones: adrenaline (肾上腺素) and noradrenaline (去甲肾上腺素). Widely distributed, being responsible for control of the stimulation and relaxation of muscle, including the heart. Mediate the control of cardiac function by the sympathetic nervous system; the parasympathetic nervous system control is mediated by muscarinic acetylcholine receptors. Remember that cytoplasmic [Ca2+] regulates the development of tension in muscles, such as the heart. 29 Case study Adrenoceptor and control of cardiac function The activation of and adrenoceptors usually elicits opposing responses: receptor activation leads to constriction of veins and arterioles. receptor activation leads to dilation of veins and arterioles. 30 Function of adrenoceptors in heart & vascular system Epinephrine administered rapidly intravenously has a number of simultaneous effects that contribute to a rapid rise in blood pressure on its administration. A rise in the strength of ventricular contraction (a positive inotropic action) The heart rate is increased (a positive chronotropic action) Blood vessels become constricted. Noting the opposing roles of and receptors, it may be no surprise to discover that administration regimes other than rapidly intravenous injection can have quite different effects. 31 1 and 2-adrenoceptor’s activation leads to constriction of vascular smooth muscle 1 and 2-adrenoceptor’s activation leads to Ca2+ influx, relaxation of vascular smooth muscle, so enhances contraction and increase heart rate. 3 and 4-adrenoceptor’s presence in heart is not fully established, and their role is even more uncertain. 32 1-adrenoceptor agonists Treat hypotension through vasoconstriction, leading to increased blood pressure. Also valuable adjuncts to local anaesthetics, as vasoconstriction can slow the systemic dispersal of the anaesthetic. Drugs in this class include: Phenylephrine Methoxamine 33 2-adrenoceptor agonists Treat hypertension, through action at the CNS, reducing signal to the heart and so lowering cardiac activity and constriction of the peripheral vasculature. Drugs in this class include: Methyldopa Clonidine 34 -adrenoceptor agonists Treat hypotension, cardiac arrhythmias & cardiac failure. Stimulate the rate and force of cardiac contraction, and lead to a drop in peripheral vascular resistance. Drugs in this class include: Xamoterol Dobutamine 35 1-Adrenoceptor antgonists Inhibiting the action of endogenous vasoconstrictors, resulting in vasodilation of both arteries and veins, and thus reduction of blood pressure. Treating hypertension and cardiac failure. Drugs in this class include: Prazosin Indoramin 36 2-Adrenoceptor antgonists Just as 2-adrenoceptor agonists unexpectedly reduce vasoconstriction and lower cardiac activity, their antagonists cause a rise in blood pressure. Yohimbine is an 2- adrenoceptor antagonist. Yohimbine 37 -Adrenoceptor antgonists Treating hypertension, angina and ischemic heart disease, also cause an increase in peripheral resistance to blood flow, although this effect is reversed on prolonged administration. Drugs in this class include: Propanolol Metoprolol 38 Projects Q&A! 1. Biological pathway simulation 2. Computer-aided anti-cancer drug design 3. Disease-causing mutation on drug target Any questions? Thank you! 39


![Shark Electrosense: physiology and circuit model []](http://s2.studylib.net/store/data/005306781_1-34d5e86294a52e9275a69716495e2e51-300x300.png)