Continued…
advertisement

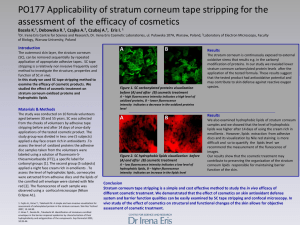
In Vivo and In Vitro Bioavailability Assessment of Topical Corticosteroid: Applications in Pharma Industry Muhammad Qamar- uz- Zaman Assistant Professor, Department of Pharmacy, The Islamia University of Bahawalpur. Objectives: Topical formulations In vivo and In vitro methods used for topical corticosteroids formulations (ointments & Creams). Applications of these studies in Pharma industry. Topical Formulations? • Prescribed to apply the drug on the skin surface to get local or systemic therapeutic effects. e.g: Ointments, Creams, Lotions, Transdermal patches etc. Need of Bioavailability studies (Topical Corticosteroids) Bioavailability leads to Bioequivalence studies to rank the relative pharmacological activities of the plethora of available commercial corticosteroids. Skin Structure Human Skin (epidermis) Bioavailability studies Two types of studies are: In vitro Modified Franz cell method In vivo Tape stripping method Skin Blanching method HPLC method Franz Cell Continued….. (Franz Cell) Test Procedure (Franz Cell) Materials: Synthetic hydrophobic polyvinylidene difluoride membrane (Durapore HVHP type, Millipore, Massachusetts) Commercially available formulation of 0.05% betamethasone dipropionate (Ointment or Cream) Modified Franz Cell Continued….. Synthetic membrane is placed on the modified Franz cell over 30 hrs Franz Cell has 1.76-cm2 orifice HVHP filter with 25 mm in diameter and 140 μm in thickness, 0.45 μm pore size & 75% porosity A Plexiglas ring is placed on the membrane Ring with internal diameter of 1.6 cm and a thickness of 0.5 cm Ring is filled with 1 mL of 0.05% betamethasone dipropionate formulation commercially available formulation (Ointment or Cream) Continued….. Drug is moved from donor compartment to receiving compartment through synthetic membrane Collect the sample from receiving compartment and perform the analysis by HPLC method to calculate the drug content Continued…. Precautions: • The hydrophobic membranes used in the drug release experiments are presoaked 5 minutes in either isopropyl myristate (IPM) or a 40:60 mixture of PEG 400: water prior to mounting on the modified Franz Cell. • Thorough contact between the membrane and the formulation is visually confirmed by viewing the underside of the membrane. • 40:60 (v/v) PEG400:water is used as vehicle as compare to water or phosphate buffered saline (pH 7.4). • The drug dose applied to the synthetic membrane is 0.28 mg of betamethasone dipropionate / cm2 In Vivo Methods Tape stripping method Skin Blanching method High Performance Liquid Chromatography (HPLC) method Tape Stripping Human Skin Continued…… Tape Stripping Human Skin Method: This approach is based on the assumption that effective cutaneous therapy requires partitioning of the topically applied drug from its vehicle formulation into the stratum corneum The amount of drug partitioning into stratum corneum can be objectively assessed by tape stripping the same and chemically quantitating the amount of drug in the tape strips. Procedure: 0.05% betamethasone dipropionate is applied to the same human subject forearm at the same time on the right and left forearms under occlusion for 24 hours. 160 mg dose is placed in a 1.2-cm diameter Hilltop chamber and affixed via the supplied adhesive tape to a 1.13 cm2 surface area on the volar aspect of the forearms. This dose, approximately 142 mg of formulation/ cm2 Continued…. Continued…. A maximum of 3 chambers, equally spaced 2cm apart, are applied to each forearm for each study, at least 6 cm above the wrist and 6 cm below the antecubital fossa to minimize the disturbance of the drug treatment throughout normal daily activity. All experimental skin site are maintained under occlusion for 24 hours. Continued… After 24 hours of treatment, the chamber is removed, and residual formulation on the skin surface is gently removed with a Teflon spatula. (The drug treated site is gently wiped with three dry cotton applicators and allowed to air dry for 1-3 minutes). Ten individual 0.6 cm diameter disks of tape are utilized to tape strip the center of the 1.2 cm diameter drug treated skin site. The sequential tape strips are combined and extracted in clean, labeled 1.5mL polypropylene microcentrifuge tubes with 200 μL of acetonitrile. Continued… The tubes are capped and vortexed for 1minute at high speed and centrifuged at 5000 rpm for 5 minutes. The supernatant is transferred into clean, labeled microcentrifuge tubes, 20 μL is injected into HPLC . A single extraction of the tape strips containing drug and stratum corneum is sufficient to routinely recover > 90% of the drug. Continued… HPLC conditions: • Retention time: 6.45 min • Column: C18 reverse phase column • Temperature: 25 centigrade • Flow rate: 1.2 mL/min • Mobile phase: acetonitrile: distilled water (65:35v/v) • Detector: UV at 254 nm Continued…. Precautions: Assessment of the amount of drug could be extremely variable due to the differences in the amount of stratum corneum removed. One approach to normalize the drug content in the tape strips among the individuals tested is to divide the drug content by the amount of tissue removed, thus giving a drug concentration, milligram of drug per milligram of stratum corneum. The amount of stratum corneum removed with the tape stripping method can be determined by weighing the tape strips before and after tape stripping. Skin Blanching Assay • Bioequivalence of topical corticosteroids from commercial cream and ointment formulation is currently assessed with Skin Blanching Assay. • Assay is Subjective • Skin blanching is monitored in the remaining drug treated skin site after tape stripping. • Skin blanching is score using 0-4 scale by a single investigator at 1, 24, and 48 hours after drug removal. Continued… • The practicality has been enhanced by combining the effects of time and skin blanching into a composite skin blanching score. • The skin blanching score that is utilized in correlation study assumes that the greater the amount of drug remaining in the skin over time, the more prolonged is the pharmacological effect. Continued… • The skin blanching score is therefore calculated additively using the time interval of observation (hours) multiplied by the extent of skin blanching at that time interval. For example: an extent of skin blanching at 1, 24, 48 hours of +4, +3, and +1, respectively, produces a score of 124: [(1) x (+4) + (24) x (+3) + (48) x (+1)] = 124. Skin blanching Scoring System Extent of Skin Blanching Description 0 No blanching 1 Slight, diffuse blanching with indistinct outline More Intense blanching with half of the treated site perimeter outline 2 3 4 Marked blanching with a distinct outline of the treated site Extreme blanching with a distinct outline of the treated site Applications in Pharma Industry In developing generic product development To meet the regulatory requirements. Helpful tool to enhance the promotion of medicines. marketing and Thank you