5. TUBULAR SECRETION
advertisement
TUBULAR SECRETION
Lecture-5
Dr. Zahoor
1
Objectives –Tubular Secretion
Define tubular secretion
Role of tubular secretion in maintaining K+
conc.
Mechanisms of tubular secretion.
2
URINE FORMATION
• Three Basic Mechanisms (Renal Processes) Of
Urine Formation include:
1. Glomerular Filtration
2. Tubular Reabsorption
3. Tubular Secretion
3
TUBULAR SECRETION
Tubular Secretion is transfer of substances
from the peritubular capillaries (capillaries
surrounding the tubule) into the tubular
lumen.
It helps to eliminate the compounds from the
body
4
Tubular Secretion
• First step is simple diffusion from peritubular
capillaries to interstitial fluid
• Entry from interstitial fluid to tubular cell can
be active or passive
• Exit from tubular cell to lumen can be active or
passive
• Examples: potassium, hydrogen, organic acids,
organic bases, NH3
5
Calculation of Tubular Secretion
Secretion = Excretion - Filtration
H+, K+, NH3
Organic acids
and bases
6
Tubular Secretion
Tubular secretion is important for:
Disposing of substances not already in the
filtrate
Eliminating undesirable substances such as urea
and uric acid
Getting rid of excess potassium ions
Controlling blood pH by secreting H+
7
TUBULAR SECRETION
The most important substances secreted are
- Hydrogen ion
- Potassium ion
- Para Amino Hippuric acid ( PAH)
- Organic anion and cations
- Drugs e.g. penicillin, aspirin, Cemitidine
- Hormones e.g. erythropoietin, renin
8
TUBULAR SECRETION
Hydrogen Ion Secretion:
Hydrogen Ion Secretion is important in acid base
balance
Hydrogen ion is secreted in the tubular lumen
and eliminated from the body in the urine
H+ ion is secreted in proximal, distal, and
collecting tubule
We will discuss H+ ion secretion in detail with acid
base balance.
9
TUBULAR SECRETION
Potassium Ion Secretion:
K+ ion secretion is controlled by aldosterone
98% of K+ is intracellular (ICF – K = 140meq/l)
ECF – K+ = 4meq/l
Slight changes in ECF – K+ can affect the
membrane excitability, therefore, plasma K+
concentration is tightly controlled by the
kidneys
10
TUBULAR SECRETION OF K+
K+ is actively reabsorbed in PCT
Na+ is actively reabsorbed and K+ is actively
secreted by principal cells in the distal and
collecting tubules and controlled by
Aldosterone.
Intercalated cells in DCT and CT actively
secrete H+ and K+ ion
Intercalated cells work for acid base balance
11
Potassium handling by nephron
MECHANISM OF K+ SECRETION
K+ is secreted in the principal cell of DCT and
CT. It is coupled to Na+ reabsorption by
energy dependent basolateral Na+ - K+ pump
13
K+ ion secretion
14
Principle cells in Late DCT
& CT
CONTROL OF K+ SECRETION
Most important control mechanism for K+ secretion
is by aldosterone
Aldosterone causes Na+ reabsorption and K+
secretion by principal cells
Increased K+ concentration directly stimulates the
adrenal cortex to increase aldosterone secretion
Decreased K+ concentration in plasma – causes
decreased aldosterone secretion
NOTE – Aldosterone secretion by Na+ is through ReninAngiotensin Aldosterone mechanism
16
Control Of
Aldosterone
Secretion By
K+ and Na+
17
Sodium Reabsorption
18
Mechanism of Aldosterone Action
Aldosterone :
Aldosterone causes Na+ re absorption and K+ secretion by
principle cell
Aldosterone causes increased Na+ entry through luminal
membrane into principal cells
Aldosterone causes Na+ pumping out of principal cells by
Na+-K+ pump into interstial fluid at basolateral membrane
Aldosterone causes K+ entry into the cell by Na+ - K+ pump,
it increases the concentration of K+ in the cell, which is
driving force for K+ secretion (passively)
19
Changes in Distal K+ Secretion
Causes of increased
Causes of decreased
Distal K+ Secretion
Distal K+ Secretion
- High K+ diet
- Low K+ diet
- Hyperaldosteronism
- Hypoaldosteronism
- Alkalosis
- Acidosis
- Thiazide diuretics
- K+ - sparing diuretics
- Loop diuretics
NOTE
Hyperaldosteronism – Hypokalemia
Hypoaldosteronism – Hyperkalemia
20
EFFECT OF H+ SECRETION ON K+
SECRETION
During acid base regulation, intercalated cells
in DCT secrete either K+ or H+
When there is acidosis, H+ ions secretion is
increased and K+ secretion is decreased
This decreased secretion of K+ leads to K+
retention in the body fluids, therefore, in
acidosis, there is hyperkalemia {increased K+}
21
IMPORTANCE OF REGULATING PLASMA
K+ CONCENTRATION
K+ plays important role in membrane
potential
K+ changes in ECF, when there is increase or
decrease in K+ level, it can affect the heart
and can cause decreased cardiac excitability,
decrease conduction, cardiac arrhythmia,
fibrillation
K+ changes not only affects cardiac muscle
but it also affects skeletal muscle and nerve
conduction
22
EFFECT OF DECREASED K+
Decreased K+ causes hyperpolarization,
which decreases the excitability of the nerve
In Skeletal muscle, K+ depletion causes
muscle weakness
K+ depletion causes abdominal distension
due to smooth muscle dysfunction
23
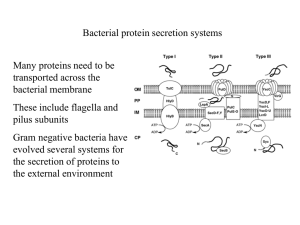
Organic Anion and Cation
secretion
Proximal tubule contains two types of secretory
carriers
For organic anions
2. For organic cations
1.
Organic ions such as Prostaglandin, epinephrine –
after their action removed from blood
Non filterable organic ions also removed
Chemicals, food additives, non nutritive
substances
Drugs – NSAID, antibiotics
PAH –EXAMPLE OF SECRETION
PAH is an organic acid
Used for measurement of renal plasma flow
Both filtered and secreted
PAH transporters located in peritubular
membrane of proximal tubular cells.
Thank you
26