Breastfeeding Education for Physicians: The Road
advertisement
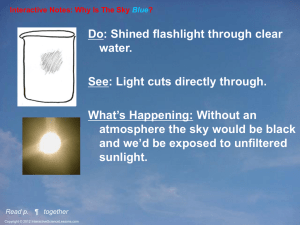
DISCLOSURES Faculty Disclosure and Resolution of Conflicts of Interest As a provider of Continuing Medical Education accredited by the Accreditation Council for Continuing Medical Education, the USCSOM-PH CME Organization must ensure balance, independence, objectivity, and scientific integrity in all its educational activities. In addition, we must show that everyone who is in a position to control the content of an educational activity has disclosed their relevant financial relationships with any commercial interest and that any conflicts of interest have been resolved. Therefore, we require that all persons in a position to control the content of this educational activity (planning committee members, moderators, faculty, etc) complete a Financial Disclosure Statement. In addition, speakers must agree to: 1. Address the specified objectives; 2. Deliver balanced evidence-based content; 3. Present the source and type or level of evidence to participants; 4. Discuss all reasonable clinical alternatives when making practice recommendations; and 5. Disclose off-label/investigative uses of commercial product/devices. Speakers who agree to participate in the activity who disclose that they have a relevant financial relationship are required to attest that: 1. These relationships will not bias or otherwise influence their involvement in the activity, and 2. Practice recommendations they make relevant to the companies with whom they have relationships will be supported by the best available evidence or, absent evidence, will be consistent with generally accepted medical practice. In addition, conflicts of interest are assessed and resolved through a review process conducted under the direction of the USCSOM-PH CME Organization. Therefore, the following disclosures are made: 1. Drs. Amrol, Krotish and Mr. Kojo Danquah-Duah disclose that neither they nor their spouses/partners have had any relevant financial relationships in the past 12 months with any proprietary entities producing, marketing, reselling, or distributing healthcare goods and services. Accreditation and Educational Credit The University of South Carolina School of Medicine-Palmetto Health Continuing Medical Education Organization designates this enduring material for a maximum of 1 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This CME Activity is planned and presented in accordance with all ACCME Essential Areas and Elements (including the Standards for Commercial Support) and Accreditation Policies. Relevant financial relationships and acknowledgements of commercial support will be disclosed to participants. Faculties are required to disclose off-label/investigative uses of commercial products/devices. Breastfeeding Education for Physicians: The Road to Baby Friendly Designation Jennifer Amrol, MD Assistant Professor of Clinical Pediatrics University of South Carolina School of Medicine Objectives Review the anatomy and physiology of breastfeeding. Examine the composition of human milk and the significance of individual components. Breast Anatomy Breast Mammary tissue Alveoli Ducts Nipple and Areola Supporting connective tissue and fat, blood and lymphatic vessels, nerves Adipose tissue distribution greatly differs among women and is not related to milk production Breast Anatomy Mammary tissue Alveoli Small sacs of milk secreting and storing cells clustered into lobules Surrounded by myoepithelial cells which contract in response to oxytocin for milk ejection Ducts Connect lobules to form distinct mammary lobe Then connect lobes to end at the galactophore Ducts beneath areola become fuller due to oxytocin during a feed Number is not related to milk production Breast Anatomy Nipple Has an average of 9 milk ducts passing to outside Has smooth muscle fibers and sensory nerves Shape and size vary between women Inverted Nipples Women with inverted nipples can breastfed but they many need more help postpartum. She should request assistance with breastfeeding as soon as possible after her baby is born. After delivery, a breast pump might be useful to help evert the nipples. If a pump is not available, a 20ml syringe with the adaptor end cut off and the plunger inserted backwards is used to help draw out a nipple. Avoid bottle and pacifier use so the baby does not become accustomed to the longer artificial nipple which feels and flows differently. When all else fails, an ultra-think silicone nipple shield can be tried temporarily. Nipple preparation during pregnancy is not recommended. Breast Anatomy Areola Circular and pigmented Contains Montgomery glands Secrete a bacteriostatic, oily fluid to protect the areola and nipple during lactation Produces the mother’s scent that attracts the baby Shape and size vary between women Stages of Lactation Mammogenesis Growth of the breasts In utero, prepubertal, pubertal Lactogenesis Functional change of the breasts so that they can secrete milk Occurs during pregnancy and initial postpartum period Galactopoiesis Maintaining the production of milk Begins 9 days postpartum Involution Termination of milk production With weaning Mammogenesis In utero Mammary bulb is seen at 18-19 weeks gestation Fat pad precursor develops Rudimentary ductal system is present at birth After birth/before puberty Small set of branching ducts grows with child Remains inactive Mammogenesis Puberty -Thelarche Takes 3 to 3 ½ years Occurs 2 ½ to 3 years prior to menarche Initial stages Increase in size and pigmentation of areola Development of breast bud Mammogenesis Puberty -Thelarche Estrogen Breast tissue enlarges Stimulates growth of mammary ducts into preexisting fat pad Progesterone Effect begins with onset of menses and ovulation Secreted by ovary during luteal phase (second half of menstrual cycle) Stimulates lobulo-alveolar development Alveolar clusters grow with each luteal phase and regress with onset of menses and loss of hormones Lactogenesis Mammary gland develops capacity to secrete milk Includes all steps needed to transform undifferentiated breast tissue in early pregnancy to fully differentiated state after pregnancy Two stages Beginning at the twelfth week of pregnancy Beginning shortly after delivery Lactogenesis Stage 1 Occurs by mid pregnancy Pregnancy hormones Progesterone Lactogenic hormones Prolactin and Human placental hormone Stimulate nipple and areolar growth Breast changes Double in weight Increased blood flow Growth in lobules and alveoli (progesterone effect) Increased secretory activity Mammary gland becomes competent to secrete milk Alveoli accumulate colostrum Colostrum is secreted immediately postpartum when the newborn feeds Milk secretion is prevented by elevated levels of estrogen and progesterone Lactogenesis Stage 2 Occurs whether or not the newborn breastfeeds Day 2 or 3 to day 8 after birth Average of 40 hours postpartum Earlier in multiparous women Tight junction in alveolar cell closes Onset of copious milk secretion Drop in levels of estrogen and progesterone Relative increase in prolactin levels Breasts are full and warm Switch from endocrine to autocrine control Continued milk production depends on regular milk removal Lactogenesis Stage 2 Blood flow, oxygen, and glucose uptake increase Progesterone Removal of placenta with its progesterone is required for milk secretion Progesterone receptors appear to be lost in lactating tissues so that the inhibitory effect of circulating progesterone is decreased once lactation is established So progesterone only birth control can be used once lactation is going well Insulin, GH, cortisol, and PTH Maternal secretion allows for mobilization of nutrients and minerals required for lactation Galactopoesis Begins 9 days after birth and continues until weaning Established milk secretion/production is maintained Continued autocrine system of control Prolactin Required to maintain milk secretion Oxytocin Required to produce let-down to allow milk extraction Involution Begins at weaning Regular milk extraction ceases Prolactin is withdrawn Is completed ~40 days after last breastfeeding Milk secretion decreases due to the buildup of inhibitory peptides Mammary gland returns nearly to pre-pregnancy state Lactation The cyclical process of milk synthesis and secretion Occurs with the help of prolactin and oxytocin Regulation of milk synthesis Quite efficient Average of ~800 ml/day but volume secreted may vary depending on infant’s requirement Milk production Improves with relaxation Decreases with maternal stress and fatigue Increased dopamine and/or norepinephrine inhibit prolactin synthesis Stress and fatigue inhibit oxytocin release Effect of Alcohol Lower levels may enhance milk letdown due to decreased stress but higher doses inhibit oxytocin release thereby inhibiting letdown Physiology of Lactation Physiology of Lactation Prolactin Polypeptide hormone synthesized in the anterior pituitary Positive regulation of secretion Released from anterior pituitary with the peak determined by the intensity of suckling by the infant Negative regulation of secretion Main control is from hypothalamic inhibitory factors (dopamine acts through the D2 receptors in lactotrophs) Stimulates mammary gland ductal growth and epithelial cell proliferation Stimulates milk synthesis in mammary gland epithelial cells Suppresses ovulation Physiology of Lactation Prolactin Levels increase from 10 ng/ml in prepregnant state to ~200 ng/ml at term Secretion occurs 7 to 20 times per day with peaks of up to 75 minutes Peak is superimposed on continuous background level of secretion Levels quickly rise with suckling and peak ~30 minutes after start of a feed Effect on milk production is most pronounced in first few weeks after birth Levels are not proportional to milk secretion and do not directly regulate milk synthesis or secretion More is produced at night so nocturnal feeds are helpful in keeping up supply Makes mother feels relaxed and sleepy Physiology of Lactation Physiology of Lactation Oxytocin Synthesized in hypothalamus and stored in the posterior pituitary Release is stimulated by suckling Neuroendocrine reflex has a significant psychological component Oxytocin release may be stimulated by thought, sight, or sound of infant Stimulates myoepithelial cells in alveoli to contract and expel milk Forcible milk removal is called milk ejection or let-down Variation in perception of let-down Aids in uterine involution after delivery Uterine contractions may be associated with “after pains” that indicate oxytocin release Physiology of Lactation Signs of Oxytocin Release Tingling sensation in breast before or during a feed Milk flowing when mother thinks of baby or hears crying baby Milk flowing from other breast during feeding Milk streaming from breast if latch is interrupted Slow deep sucks and swallows by the baby during feed Uterine pain during feed Thirst during a feed Physiology of Lactation Milk production Positive local regulation by demand 1. 2. 3. Increased suckling Increased emptying Increased milk secretion/production Skin to Skin (SSC) supports successful breastfeeding Partial milk removal sets a new, lower rate of milk production Negative local regulation of milk production Feedback Inhibitor of Lactation Accumulates in milk between feeds so without removal of milk, secretion/production is inhibited Explains why an empty breast makes milk faster than a fuller one Distention or stretch of the alveoli Local effect to inhibit milk secretion/production Once milk removal stops, involution begins Physiology of Lactation Feedback Inhibitor of Lactation Inhibitory whey protein present in breast milk Builds up as milk accumulates in the mammary gland Without milk removal, the inhibitor stops epithelial cells from secreting/producing more milk Protects breast from harmful effects of overfilling Once milk is removed, secretion restarts Allows production of milk to be determined by infant’s needs Especially important regulatory mechanism once lactation is established since prolactin does not control milk volume produced Maternal Diet and Milk Supply Mothers make nourishing milk for their infants from all kinds of food. There are no foods that must be avoided, unless mother or baby develops an allergic reaction. Breastfeeding mothers have an increased thirst that usually maintains an adequate fluid intake; no data support the assumption that increasing fluid intake will increase milk volume. Mothers do not need to drink milk to make milk; thirst can be satisfied from a variety of nourishing beverages, including water. Calcium is available not only in milk and milk products but in many other foods, such as broccoli, spinach, kale, bok choy, collards, mustard and turnip greens, almonds, and canned fish. Poor maternal nutrition is not a contraindication to breastfeeding. Mothers following a vegan diet should take a B12 supplement Galactagogues Metoclopramide — most commonly used Domperidone — not approved in USA. Similar to metoclopramide but less side effects as little crosses blood brain barrier Fenugreek and other herbal medicines — no scientific data except anecdotal reports Goat’s rue, milk thistle, anise, basil, blessed thistle, fennel seeds and marshmallow Metoclopramide Effect is to increase prolactin level Benefit shown in small placebo controlled crossover study with increase of 50 cc per feed with dose of at least 30 mg per day Side effects gastrointestinal, anxiety, sedation, and rare dystonic reactions No documented neonatal reactions Short term: 1–3 weeks is common. No evidence supporting long-term use. Usually wean after 10–14 days Common dosing regimen 10 mg po qd first day Then 10 mg po bid Then 10 mg po TID Fenugreek Most commonly recommended herbal galactogogue Usual dose is 1-4 capsules (580-610mg) tid to qid No standard dosing May also be taken as one cup of strained tea tid ¼ tsp seeds steeped in 8oz water for 10 minutes Increases supply within 24 to 72 hours Side effects in mother Maple like odor to sweat, milk, and urine Diarrhea Increased asthmatic symptoms Lower blood sugar Contraindicated during pregnancy due to uterine stimulant effects Human Milk Composition Human Milk Composition Colostrum Denser milk provided for the first 2-3 days after birth Facilitates the passage of meconium to decrease enterohepatic circulation and thus encourage elimination of bilirubin Aids in establishment of Lactobacillus bifidus flora in infant’s gut Milk Volumes Day 1 40-50 ml (range of 7-123ml) Day 3 300-400 ml Day 5 500-800 ml Low volumes encourage frequent feeds to stimulate milk synthesis Colostrum Energy Value 67 kcal/100ml Colostrum components Higher concentrations of Na, K, and Cl than mature milk Higher percentage of protein, minerals and fat soluble vitamins than mature milk Human Milk Composition Colostrum Denser milk with higher concentration of proteins White cells and antibodies (especially sIgA) Important immune protection from exposures to environmental microorganisms 40-60% of cells are macrophages Epidermal growth factor Prepares gut lining to receive nutrients in milk Lactose Prevents hypoglycemia and facilitates meconium passage and therefore bilirubin excretion Vitamin A Protects the eyes and epithelial surfaces Beta carotene, its precursor, provides yellowish color of colostrum Human Milk Composition Immunoglobulins in Human Milk (levels decrease over time) Day Postpartum 1 3 7 8 – 50 Output - mg/24 hours IgG IgM IgA 80 120 11,000 50 40 2,000 25 10 1,000 10 10 1,000 Human Milk Composition Note the increases in calories, lactose, and fat while the protein decreases from colostrum to mature milk. Human Milk Composition Transitional Milk Milk produced from days 5-12 Intermediate composition between colostrum and mature milk Volume continues to increase Macrophage as percentage of WBCs increases to 80-90% Concentration is 104 to 105 per ml of milk Human Milk Composition Mature Milk Milk produced after ~14 days Contains all the nutrients an infant needs for the first 6 months of life and is uniquely specific for humans Fat (3.8%), protein (0.9%), carbohydrates (7.2%), vitamins, minerals, and water (87%) Is easily digested and efficiently used Composition varies through lactation: over a day, within a feed, and between women Calories 20 calories per ounce (65-75 kcal/100ml) Formula Milk Breast Milk Note the substantial structure of human milk under a microscope; this is due to the compartmentation of the various components such as the nutrients and bioactive substances. This image demonstrates that milk is a living tissue containing about 4000 cells/cubic mm including neutrophils, macrophages, and lymphocytes. Human Milk Composition Water Human milk is 87% water Provides sufficient fluid to maintain hydration even in hot climates Human Milk Composition Fat Fat content 3.5-3.8g/100ml provides 50% of energy/calories in milk Most variable component of human milk Separates on standing Contains cholesterol, triglycerides, short-chain fatty acids, and long-chain polyunsaturated fatty acids Foremilk Milk that accumulates in breast since previous feed Lower fat content (1.5 to 2%) and looks bluish-gray Hindmilk Milk that is secreted during a feed Higher fat content (2-3x more than foremilk- 5 to 6%) and looks creamy white Human Milk Composition Fat content increases from the start of a feed (~1.7%)to the end of a feed (~5.5%). Protein content decreases from the start (0.9%) of a 7.0 feed to the end (0.7%). 6.0 Foremilk has less fat but more protein than hindmilk. 5.0 4.0 Fat 3.0 Protein 2.0 1.0 0.0 Foremilk Hindmilk Human Milk Composition Fat Lipid Component Milk fat globule Forms with lipid secretion from apical mammary epithelial cell and envelopment in its plasma membrane Also contains proteins, growth factors, and vitamins Mucins on the globule membrane adhere to viruses and bacteria to aid in elimination from body Human Milk Composition Fat Lipid Component Bile salt-stimulated lipase Acts on triglycerides to produce free fatty acids and 2-monoglycerides Prevents fatty acids from forming soaps with minerals Results in superior absorption of fat and minerals Not present in formula Human Milk Composition Fat Lipid Component Abundance of essential fatty acids (linoleic and linolenic acids) Most exist as triacylglycerols and phospholipids 167 fatty acids have been identified in human milk Unique long chain polyunsaturated fatty acids (including omega-3 fatty acids DHA and ARA) Term infants are able to convert long chain polyunsaturated fatty acids to DHA and ARA so the addition of these to term formulas may be unnecessary but is likely useful for preterm infants who cannot convert them. Cholesterol is also present in significant quantities Human Milk Composition Protein Human milk contains 9g protein/L (whey and casein) Less than in other animal milks Whey proteins consist primarily of α-lactalbumin without β-lactalbumin Cow milk whey contains β-lactalbumin to which infants can become intolerant Contains less casein than other milks Provides 80% of milk’s nitrogen Protein content declines over 2-4 weeks but then is constant until weaning Human Milk Composition Protein Colostrum 90/10 ratio of whey/casein Mature Milk 70/30 ratio of whey/casein Late Lactation 50/50 ratio of whey/casein Cow Milk 18/82 ratio of whey/casein Human Milk Composition Protein Whey (70%) Contains water, electrolytes, and proteins α-lactalbumin, albumin, lactoferrin, immunoglobulins, enzymes (e.g., lysozyme), growth factors, and hormones Remains in solution after acidification Lactoferrin, lysozyme, and sIgA resist proteolytic digestion and line the GI tract to provide host defense Present only in human milk Generally more easily digested and associated with more rapid gastric emptying Human Milk Composition Protein- Whey Lactoferrin Transports and promotes the absorption of iron Inhibits the growth of iron-dependent bacteria in the gastrointestinal tract such as coliforms and yeast Lysozyme Enzyme that protects the infant against E. Coli and Salmonella Promotes the growth of healthy intestinal flora and has antiinflammatory functions Secretory IgA Primary Ig in breastmilk Protects the infant from viruses and bacteria, specifically those to which the baby, mom, and family are exposed Helps protect against E. Coli Human Milk Composition Protein Casein (30%) β-casein forms a soft curd in the infant’s stomach if pH<5 Curd is an insoluble calcium caseinate-calcium phosphate complex Low solubility in acid Human milk casein curds are more easily digested than those in other milks Human Milk Composition Non-protein nitrogen containing compounds Provide 20% of nitrogen in milk Epidermal growth factor Contributes to the development and function of intestinal mucosa Taurine Free amino acid associated with bile acid conjugation and neurotransmission Nucleotides Have metabolic and immune functions Carnitine Used for lipolysis of long-chain fatty acids Somatomedin-C, Insulin and other peptides Human Milk Composition Carbohydrates When is lactase present in the infant gut? Present in maximal amounts in the intestinal brush border of full term infants Deficient before 34 wga Human Milk Composition Carbohydrates Lactose (90%) 7.2g/L Disaccharide of galactose and glucose synthesized in the breast Important source of glucose Important source of galactose for galactolipids used in infant brain development Monosaccharides, oligosaccharides, and glycoproteins (10%) Oligosaccharides prevent bacteria from adhering to mucosal surface Oligosaccharides plus glycoproteins = “bifidus factor” Stimulate growth and colonization of newborn’s gut with Lactobacillus bifidus (beneficial bacteria that creates an acidic gut where harmful bacteria cannot survive) Human Milk Composition Minerals Content is similar between mammal milks but concentrations, ratios, and bioavailability are species specific Lower quantities results in lower solute load for immature renal system Iron, sodium, potassium, calcium, magnesium, zinc, and small amounts of copper, selenium, chromium, manganese, molybdenum, and nickel Zinc and Iron Well absorbed from human milk Zinc deficiency is rare in breastfed infants whose mothers have adequate Zn intake Human Milk Composition Iron 100mcg/L versus formula with 12mg/L 50-100% of human milk iron is absorbed 4% of iron fortified formula iron is absorbed Absorption is enhanced by high lactose and vitamin C concentrations in human milk Lactoferrin in whey binds iron Increasing digestion and absorption of iron Also makes iron unavailable to iron dependent bacteria in gut Normal full-term infants can be exclusively breastfed for 6 months without becoming iron deficient Human Milk Composition Vitamins Vitamin A, beta carotene, and vitamin E Plentiful in colostrum and early transitional milk Vitamin A protects against infection and aids early retinal development Vitamin E protects red cells against hemolysis Vitamin D Sufficient only with adequate maternal diet and maternal and infant sun exposure AAP recommends 400 IU/d for all breastfed infants until they are ingesting or exposed to sufficient Vitamin D from other sources Vitamin K Poorly transported prenatally and also limited in human milk All newborns must receive Vitamin K at birth Vitamin B12 Mothers on vegan diets may produce B12 deficient milk so supplements are recommended Examples of the Non-nutritional Components of Human milk Antimicrobial factors secretory IgA, IgM, IgG lactoferrin lysozyme complement C3 leukocytes bifidus factor lipids and fatty acids antiviral mucins, GAGs oligosaccharides Cytokines and anti-inflammatory factors tumour necrosis factor interleukins interferon-g prostaglandins a1-antichymotrypsin a1-antitrypsin platelet-activating factor: acetyl hydrolase Transporters lactoferrin (Fe) folate binder cobalamin binder IgF binder thyroxine binder corticosteroid binder Others casomorphins d -sleep peptides nucleotides DNA, RNA http://www.unu.edu/unupress/food/8F174e/8F174E04.htm Growth factors epidermal (EGF) nerve (NGF) insulin-like (IGF) transforming (TGF) taurine polyamines Digestive enzymes amylase bile acid-stimulating esterase bile acid-stimulating lipases lipoprotein lipase Hormones feedback inhibitor of lactation (FIL) insulin prolactin thyroid hormones corticosteroids, ACTH oxytocin calcitonin parathyroid hormone erythropoietin Potentially harmful substances viruses (e.g., HIV) aflatoxins trans-fatty acids nicotine, caffeine food allergens PCBs, DDT, dioxins radioisotopes drugs Human Milk Composition Passive Immunization via the Enteromammary Pathway Maternal exposure Breast tissue and breastmilk Antigens Maternal gut Lymphoblasts Mesenteric node Infant gut Other mucosal surfaces Lymphoblasts mature into lymphocytes that produce immunoglobulins that move into the bloodstream Blood stream Thoracic duct Milk Composition Differences Human Milk Commercial Substitutes Protein Appropriate (species specific) quality/quantity, easier to digest Corrected in quantity but not in quality (not species specific) Fat Appropriate quality/quantity of essential fatty acids, lipase present Lipase absent Vitamins Adequate except for vitamins D and K in some situations Vitamins added Minerals Correct amount Partly corrected Anti-Infective properties Present Absent Growth Factors Present Absent Digestive enzymes Present Absent Hormones Present Absent Thank you for completing Section 2 of Breastfeeding Education for Physicians. To obtain CME credit, please click on the link below, provide your information and complete the post-test https://www.surveymonkey.com/s/BreastfeedingSectio n2