Conception and Fetal
Development
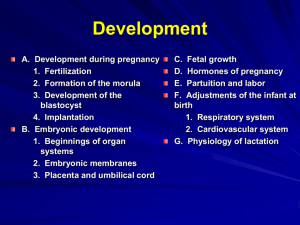
Cellular Division
• Zygote – life begins as a single cell
• Mitosis – exact copies of the original
• Meiosis – development of new organism
– Reproductive cells
Gametogenesis
• Oogenesis
–
–
–
–
Process where ovaries form ova
All ova female has is present at 6 months of life
1st meiotic division secondary oocyte and polar body
At ovulation, 2nd meiotic division begins and completes
only if fertilized
– One ovum and 3 polar bodies
• Spermatogenesis
– Process where testes produce sperm
– Replicates into two secondary spermatocytes
– 2nd meiotic division , 4 spermatids are formed
Egg
Sperm
Figure 3–1a Gametogenesis involves meiosis within the ovary and testis. During meiosis each oogonium produces a single haploid
ovum once some cytoplasm moves into the polar bodies.
Fertilization
• Preparation for fertilization
– Estrogen levels increase
– Peristalsis of fallopian tubes increases
– Cervical mucus thins to allow sperm to transfer through
• Time frame
– Ova viable for 24 hours
• Sperm
– Capacitation to expose acrosome
• Define: Capacitation- Process that removes plasma to expose the
acrosome
• Define: Acrosome- A membrane at the leading edge of a sperm cell
– Block to polyspermy “The penetration of an ovum by more
than one sperm”
• True fertilization
– When nuclei of ovum and sperm unite
Ova
Fertilization
Figure 3–2a Sperm penetration of an ovum. The sequential steps of oocyte penetration by a sperm are depicted moving from top to
bottom. Source: Scanning electron micrograph from Nilsson, L. (1990). A child is born. New York: Dell Publishing.
Sperm penetrating ova
30 Hours – Two cells
Two days – 4 visible cells
Morula stage
Four days – surrounded by
Zona pellucida
Blastocyst breaking out
of Zona Pellucida
Twins
• Fraternal
–
–
–
–
Dizygotic- derived from two separately fertilized eggs
Separate placentas, chorions, amnions (2 of each)
Not identical
Incidence increases with maternal age, in families with
genetic factors that increase amounts of gonadotropin
• Identical
– Monozygotic- derived from a single fertilized egg
– Same placenta, chorion and amnion may be the same or
different depending on when division occurs
– Same sex
– Random event
Figure 3–3a Formation of identical twins.
Figure 3–3b Formation of fraternal twins (Note separate placentas.)
Preembryonic development
1st 2 wks of development
• Cellular Multiplication
– Zygote moves through fallopian tube
– Rapid mitotic division – morula
• Define: Morula- a solid mass of blastomeres that forms when the
zygote splits
– Blastocyst develops into embryo and amnion
– Trophoblast develops into chorion
• Implantation (aka “Nidation”- fertilized egg becomes implanted in
the lining of the uterus)
– Attaches to surface of endometrium (process called, decidua)
– Occurs 7 – 9 days after fertilization
Secreting a mucus for protection
11 days – burrowed in
endometrium
Figure 3–4 During ovulation, the ovum leaves the ovary and enters the fallopian tube. Fertilization generally occurs in the outer
third of the fallopian tube. Subsequent changes in the fertilized ovum from conception to implantation are depicted.
Embryonic Membranes
• Chorion
– Outer most membrane
– Fingerlike projections, “villi”
• Amnion
– Thin protective membrane
– Contains amniotic fluid
• As embryo grows, amnion comes in
contact with chorion and forms fluid filled
sac
Amniotic Fluid
• Functions
– Protection, temperature regulation, permit
symmetrical growth, prevents adherence of
the amnion, gives freedom of movement
• Amounts
– Ranges from 700 – 1000cc’s at term
– Abn Variations:
• Oligohydramnios < than normal; Oligo- few, little
• Polyhydramnios > 2000cc’s; Poly- many
Preembryonic/Embroyonic
• Yolk Sac
– Second cavity developed at 8 –9 days
– Forms primitive RBC’s during 1st 6 weeks
• Umbilical Cord
– Formed from the amnion; attaches the embryo to the yolk sac
– Three vessels – two arteries and one vein
– Wharton’s jelly surrounds vessels in cord preventing cord
compression
– Twisted or spiraled from fetal movement
– Nuchal cord- cord is around the neck
– True knot- very rare
Lack of Jelly
Figure 3–6 Endoderm differentiates to form the epithelial lining of the digestive and respiratory tracts and associated glands. Source:
Adapted from Marieb, E. N. (1998).
3 weeks – groove of neural tube
4 weeks
5 weeks – heart & liver
5 ½ weeks
6 weeks
Placenta
There is no mixing between mom’s and baby’s blood
• Functions
– Metabolic, nutrient, and gas exchange
between embryonic and maternal circulation
• Development
– Chorionic villi – functional layer of placenta
– Anchoring villi – forms the partitions/walls called
cotyledons
– Branching villi – vascular system where gas
exchange takes place
Placental Circulation
• Metabolic gas exchange begins at 4 weeks
• Funic souffle soft blowing heard over umbilical
cord – synchronous with fetal heartbeat,
hearing bloodflow through vessel
• Uterine souffle heard just above mother’s
pelvis – synchronous with maternal pulse
• Placental bloodflow enhanced when mother
lies on left side
Placental Functions
Just know that there’s diff forms of transport
• Metabolic activities – produces glycogen, fatty
acids are more available, cholesterol,
enzymes; stores glycogen, iron
• Transport functions
–
–
–
–
–
Simple diffusion to
Facilitated transport to requires energy
Active transport to
Pinocytosis transfers large molecules by engulfing
Bulk flow results from hydrostatic and osmotic
pressure
Endocrine Functions of the
Placenta
• Human Chorionic Gonadotropin (HCG)
– Prevents normal involution of corpus luteum
– Causes corpus luteum to secrete estrogen
and progesterone
– basis for pregnancy tests
• Blood @ 8 –10 days
• Urine a few days after missed period
Placental Hormones con.
• Progesterone
– Hormone of pregnancy
– Decreases contractility of the uterus
– Maintainance/Essential for pregnancy to continue
after 11 weeks
• Estrogen
– Placenta produces 50% more
– Proliferative function – breasts and uterus
• Human Placental Lactogen
– Similar to pituitary growth hormone
– Stimulates changes in maternal metabolic
processes
– Indicator of fetal growth
(**Will be covered later)
Figure 3–11 Fetal circulation. Blood leaves the placenta and enters the fetus through the umbilical vein. After circulating through the
fetus, the blood returns to the placenta through the umbilical arteries. The ductus venosus, the foramen ovale, and the ductus
arteriosus allow the blood to bypass the fetal liver and lungs.
Embryo and Fetal Development
*40wks for pregnancy, 38wks of development
• Length of pregnancy
– 10 lunar months or 40 weeks (Full term)
– Postconception age is 38 weeks after fertilization
• Preembryonic
– First 14 days of development
• Embryonic
– Starts on day 15 and continues through 8th week
– Most vulnerable to Teratogens
Embryonic Stage
KNOW: When Hrt Beat? Size?
• 3 weeks – broad cephalic end and a narrow
caudal end; heart is most advanced organ
• 4 – 5 weeks –
– vertebrae form from somites;
– eyes and ears begin development, arm and leg
buds;
– partitioning in heart;
– brain differentiated into five areas;
– heart, brain, and circulatory system show most
development
Embryonic Stage con.
• 6-7 weeks – head structures highly developed,
arms and legs have digits, fetal circulation begins
to be established, liver produces RBC’s, eyelids
begin to form, rectal and urogenital passages
separate
• 8 weeks – resembles a human being, eyelids
fuse, external genitals appear, rectal passage
opens, long bones are forming, and large
muscles contract
Figure 3–12 The actual size of a human conceptus from fertilization to the early fetal stage. The embryonic stage begins in the third
week after fertilization; the fetal stage begins in the ninth week. Source: Adapted from Marieb, E. N. (1998).
Fetal Stage
End of 8th wk
• 9-12 weeks – head large and comprises half of fetus,
sucking reflex present, limbs are long and slender
with well formed digits, forms urine, FHT “Fetal Hrt Tones”
heard with doppler, swallows amniotic fluid,
meconium present in intestines
• 13-16 weeks – rapid growth, lanugo “fine hair” present,
moves arms and legs
• 20 weeks – weighs about 1 pound, deposits brown
fat, head covered with fine wooly hair, eyebrows,
eyelids, nails and muscles well developed, mother
feels movement quickening
Fetal Stage con.
• 24 weeks – weighs 780 gms, hand grasp and
startle reflex present, covered with vernix, alveoli
in lungs beginning to form
• 25-28 weeks – brain develops rapidly, CNS
mature enough to provide some regulatory
functions, eyelids open, weighs about 1200 gms
• 29-32 weeks – pupilary light reflex present, weighs
about 2000gms, stores iron, Ca , phosphorous
• 36 – 40 weeks – primarily weight gain
Factors Influencing Fetal
Development
• Quality of ovum or sperm
• Adequacy of uterine environment
– If unsuitable
• Cells may die abortion
• Growth slowed
• Teratogens “agent/substance which cause
malformation”; 1-8wks most vulnerable to induced
malformations
• Maternal environment
– Nutrition– 5th lunar month (20wks) to 6 months of life
– Hyperthermia– Sauna/Hot Tub during 1st trimester linked to
CNS defects
6 weeks
7 weeks
8 weeks
9 weeks
10-11 weeks
12 weeks
13 weeks – eyes are fused
15 weeks
15 weeks
Female at 18 weeks
18 – 20 weeks
22 weeks
24 weeks
32-34 weeks
36 weeks
Ready for birth