Changes in Chromosome Number
Chapter 3
Central Points
Chromosomes are composed of DNA and proteins
Most humans have 46 chromosomes
Possible to test fetal chromosome number
Extra chromosomes affect fetus
Problems with genetic testing can result in lawsuits
Case A: Results Worry Pregnant Woman
Martha, age 41, is 18-weeks pregnant
Increased risk of chromosomal abnormalities
Amniocentesis recommended
Test results:
• No Down syndrome
• Fetus is XYY (Jacobs syndrome)
XYY Karyotype
3.1 Chromosomes
Thread-like structures in
nucleus
Carry genetic information
Humans have 46
Parts
•
•
•
•
Centromere
p arm
q arm
Telomeres
p arm
Centromere
q arm
Fig. 3-1, p. 43
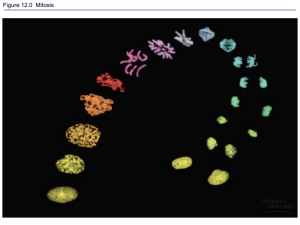
Animation: How Cells Reproduce
(chromosome structure and organization)
3.2 Changes in Chromosome Number
Eggs and sperm are produced by meiosis
Begin with two copies of each chromosome (46)
Two divisions meiosis I and meiosis II
Homologous chromosome pairs separate
Produces haploid cells with one copy of each
chromosome (23)
Meiosis: Produces Haploid Cells
Before cells begin meiosis, the chromosomes duplicate.
As meiosis begins, chromosomes coil and shorten, and
become visible in the microscope. Each chromosome
has a matching partner and the two chromosomes may
exchange parts (cross over) during this stage, called
prophase I.
p. 44
The chromosome pairs line up along the
middle of the cell, and spindle fibers attach
to the centromere of each pair. This stage is
called metaphase I.
p. 44
Members of each homologous pair separate
and move toward opposite sides of the cell.
This stage is called anaphase I.
p. 44
The chromosomes reach opposite poles of the cell,
and the nuclei begin to re-form. This stage is called
telophase I. The cytoplasm divides, and two cells
are formed. These cells have half the number of
chromosomes of the original cells and are called
haploid cells.
p. 44
MEIOSIS I
Before cells begin
meiosis, the
chromosomes duplicate.
As meiosis begins,
chromosomes coil and
shorten, and become
visible in the
microscope. Each
chromosome has a
matching partner and
the two chromosomes
may exchange parts
(cross over) during this
stage, called prophase I.
The chromosome
pairs line up along
the middle of the
cell, and spindle
fibers attach to the
centromere of each
pair. This stage is
called metaphase I.
Members of each
homologous pair
separate and move
toward opposite
sides of the cell. This
stage is called
anaphase I.
The chromosomes reach
opposite poles of the cell,
and the nuclei begin to
re-form. This stage is
called telophase I. The
cytoplasm divides, and
two cells are formed.
These cells have half the
number of chromosomes
of the original cells and
are called haploid cells.
Stepped Art
p. 44
Meiosis: Produces Haploid Cells
Two cells formed
during meiosis I. In
prophase II, the
chromosomes of
these cells become
coiled, and move
toward the center of
the cell.
p. 44
The 23 chromosomes
in each cell attach to
spindle fibers at their
centromeres. This
stage is called
metaphase II.
p. 44
Each centromere
divides, and the
newly formed
chromosomes (also
called sister
chromatids) move to
opposite ends of the
cell. This stage is
called anaphase II.
p. 44
Finally, the
chromosomes uncoil
and the nuclear
membrane re-forms.
This stage is called
telophase II. After the
cytoplasm divides,
the result is four
cells, each with the
haploid number of
chromosomes.
Meiosis is now
completed.
p. 44
MEIOSIS II
Two cells formed
during meiosis I. In
prophase II, the
chromosomes of
these cells become
coiled, and move
toward the center of
the cell.
The 23 chromosomes
in each cell attach to
spindle fibers at their
centromeres. This
stage is called
metaphase II.
Each centromere
divides, and the newly
formed chromosomes
(also called sister
chromatids) move to
opposite ends of the
cell. This stage is
called anaphase II.
Finally, the chromosomes
uncoil and the nuclear
membrane re-forms. This
stage is called telophase II.
After the cytoplasm divides,
the result is four cells, each
with the haploid number of
chromosomes. Meiosis is
now completed.
Stepped Art
p. 44
Events in Meiosis
Animation: Meiosis
Animation: Mitosis
Nondisjunction
Chromosomes fail to separate
Results in gametes and zygote with an abnormal
chromosome number
Aneuploidy is variations in chromosome
number that involve one or more chromosomes
Most aneuploidy from errors in meiosis
Nondisjunction
Chromosome
number in gametes:
Extra
chromosome
(n + 1)
Extra
chromosome
(n + 1)
Missing
chromosome
(n – 1)
Missing
chromosome
(n – 1)
Chromosomes
align at metaphase I
Nondisjunction
at anaphase I
Alignments at
metaphase II
Anaphase II
Fig. 3-2, p. 45
Chromosome
number in gametes:
Extra
chromosome
(n + 1)
Extra
chromosome
(n + 1)
Missing
chromosome
(n – 1)
Missing
chromosome
(n – 1)
Chromosomes
align at metaphase I
Nondisjunction
at anaphase I
Alignments at
metaphase II
Anaphase II
Stepped Art
Fig. 3-2, p. 45
Aneuploidy
Effects vary by chromosomal condition
Many cause early miscarriages
Leading cause of mental retardation
3.3 ID of Chromosomal Abnormalities
Two tests:
Amniocentesis (> 16 weeks)
• Collects amniotic fluid
• Fetal cells grown and karyotype produced
Chorionic villus sampling (CVS) (10–12 weeks)
• Rapidly dividing cells
• Karyotype within few days
Amniocentesis
Removal of about
20 ml of amniotic
fluid containing
suspended cells
that were sloughed
off from the fetus
Biochemical analysis
of the amniotic fluid
after the fetal cells
are separated out
Centrifugation
Analysis of fetal cells
to determine sex
Fetal cells
are removed
from the
solution
Cells are
grown in an
incubator
Karyotype analysis
p. 46
Removal of about
20 ml of amniotic
fluid containing
suspended cells
that were sloughed
off from the fetus
Biochemical analysis
of the amniotic fluid
after the fetal cells
are separated out
Centrifugation
Analysis of fetal cells
to determine sex
Fetal cells
are removed
from the
solution
Cells are
grown in an
incubator
Karyotype analysis
Stepped Art
p. 46
Karyotype
Animation: Chromosomes and Human
Inheritance (karyotype preparation)
Chorionic Villus Sampling (CVS)
Chorionic
villi
Ultrasound to
monitor procedure
Developing
placenta
Developing fetus
Bladder
Uterus
Chorion
Catheter
Amniotic
cavity
Rectum
p. 47
Amniocentesis Only Used in Certain
Conditions
Risks for miscarriage; typically only done under
one of following circumstances:
•
•
•
•
•
Mother > 35
History of child with chromosomal abnormalities
Parent has abnormal chromosomes
Mother carries a X-linked disorder
History of infertility or multiple miscarriages
Other Chromosomal Variations
Polyploidy: multiple sets of chromosomes
Euploid: normal two copies of each chromosome
Trisomy: three copies of one chromosome
Monosomy: only one copy of a chromosome
Structural changes: duplication, deletion,
inversion, translocation
Structural Changes in Chromosomes
p. 47
Normal chromosome
One segment repeated three times
p. 47
p. 47
Segment C deleted
p. 47
p. 47
Segments
G, H, I
become
inverted
p. 47
p. 47
Chromosome A
Chromosome B
Translocation
p. 47
Animation: Chromosome abnormalities
exercise
Animation: Meiosis and Sexual
Reproduction (Meiosis I and II)
3.4 Effects of Changes in Chromosomes
Vary by chromosome and type of variation
May cause birth defects or fetal death
Monosomy of any autosome is fatal
Only a few trisomies result in live births
Autosomal Trisomies
Autosomal Trisomies
Autosomal Trisomies
Trisomy 13: Patau Syndrome (47,+13)
1/15,000
Survival: 1–2 months
Facial, eye, finger, toe, brain, heart, and
nervous system malformations
Patau Syndrome
Trisomy 13: Edwards Syndrome (47,+18)
1/11,000, 80% females
Survival: 2–4 months
Small, mental disabilities, clenched fists, heart,
finger, and foot malformations
Die from heart failure or pneumonia
Edwards Syndrome
Trisomy 21: Down Syndrome (47,+21)
1/800 (changes with age of mother)
Survival up to age 50
Leading cause of childhood mental retardation
and heart defects
Wide, flat skulls; eyelid folds; large tongues;
physical, mental, development retardation
May live rich, productive lives
Down Syndrome
Leading Risk Factor for Trisomy
Maternal age
Unknown why, older eggs increase risk of
nondisjunction
Eggs held in meiosis I from birth to ovulation
Possible changes in maternal selection
Maternal Age and Down Syndrome
Aneuploidy and Sex Chromosomes
More common than in autosomes
Turner syndrome (45,X): monosomy of X
chromosome
Klinefelter syndrome (47,XXY)
Jacobs syndrome (47,XYY)
Sex Chromosome Trisomies
Sex Chromosome Trisomies
Sex Chromosome Trisomies
Turner Syndrome (45,X)
Survival to adulthood
Female, short, wide-chested, undeveloped
ovaries, possible narrowing of aorta
Normal intelligence
1/10,000 female births, 95–99% of 45,X
conceptions die before birth
Turner Syndrome
Klinefelter Syndrome (47,XXY)
Survival to adulthood
Male
Features do not develop
until puberty, usually sterile,
may have learning
disabilities
1/1,000 males
Klinefelter Syndrome
XYY or Jacobs Syndrome (47,XYY)
Survival to adulthood
Average height, thin, personality disorders,
some form of mental disabilities, and adolescent
acne
Some may have very mild symptoms
1/1,000 male births
XYY Syndrome
3.5 Ways to Evaluate Risks
Genetic counselors are part of the health care
team
In nondirective way, they assist understanding of:
•
•
•
•
•
•
Risks
Diagnosis
Progression
Possible treatments
Management of disorder
Possible recurrence
Counseling Recommendations (1)
Pregnant women or those who are planning
pregnancy
Women > age 35
Couples with a child with:
• Mental retardation
• A genetic disorder
• A birth defect
Counseling Recommendations (2)
Couples from certain ethic groups
Couples that are closely related
Individuals with jobs, lifestyles, or medical
history that may pose a risk to a pregnancy
Women who have had two or more miscarriages
or babies who died in infancy
Genetic Counseling
Most see a genetic counselor:
• After a prenatal test;
• After the birth of a child; or
• To determine their risk
Counselor
• Constructs a detailed family history and pedigree
• Shares information that allows an individual or a
couple to make informed decisions
Case A Questions
Child is XYY: What are the best options?
Would the options change if the child had a
different condition?
Who should know?
See the textbook for further questions on this
case
Case B: Test Results Worry Doctor
31-year-old woman gave birth to a child with
serious abnormalities
Sued doctor for not performing amniocentesis
What legal issues should concern the doctor and
what should she do?
See the textbook for further questions on this
case
Future of Genetic Counseling
Human Genome Project (HGP) changed
medical care and genetic testing
Genetic counselor will become more important
Evaluate reproductive risks and other conditions
Allow at-risk individuals to make informed
choices about lifestyle, children, and medical
care
3.6 Legal and Ethical Issues
Wrongful-birth suit
Wrongful-life suit
Based on:
1. Could a diagnosis of this condition have been made
in time to have an abortion?
2. Was the condition serious enough that a reasonable
person would have had an abortion?
Wrongful-Birth and Wrongful-Life Cases
Issues with Wrongful-Birth and
Wrongful-Life Suits
Wrongful-birth suit (most states allow):
• Roe v. Wade gave a woman an alternative to
birth
• Doctors have extensive medical malpractice
insurance
Wrongful-life suits (only 5 states allow):
• Courts uncomfortable declaring someone should
never have been born
XYY Individuals (Jacobs Syndrome)
Early studies linking XYY with aggressive/
criminal behavior no longer supported by
research
Should parents and or child know the condition?
What should the doctor do?
Spotlight on Law: Becker v. Schwartz
Becker, age 37, was not informed about
amniocentesis
Child born with Down syndrome, parents sued
doctor for “wrongful life”
Parents won $2,500 and gave baby up for
adoption
What is your opinion on this case?