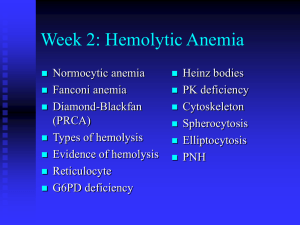
Iron deficiency anemia
advertisement

Bone marrow Red Yellow Bone Fat Reticulin Haematopoiesis – red, white, platelets lymphoid Normal red cells Central pale area Red cells Men • Hemoglobin (g/l) 140-180 • Hematocrit (%) 40-52 • Red cell count (1012/l) 4.5-6.5 • • • • Women 120-160 36-48 3.9-5.6 Reticulocyte count (%) 0.5-1.5 Mean cell volume (fl) 80-95 Mean corpuscular hemoglobin (pg) 27-33 Mean corpuscular hemoglobin concentration (gm/dL) 33-37 Red cells pathological conditions: I. decrease in the circulating red cell mass (poss. with structural abnormalities) very common - anaemia II. increase in the circulating red cell mass less common polycythemia =erythrocytosis=polyglobuly Polycythemia =increased concentration of red cells • RELATIVE - decreased plasma volume dehydration, stress • ABSOLUTE primary – neoplastic= polycythemia vera = myeloproliferative neoplasm secondary - increased erythropoietin stimulation Appropriate reactive – low levels of oxygen in the PB (heart disease, high altitude) Inappropropriate Red cells • Normal: uniform in size and shape • Pathologic: variation in size, shape, inclusions • Variation • size - anisocytosis • Shape – poikilocytosis Red cells - functions • Deliver oxygen to the tissues • • • • Anemia - reduction of the total number of red cells amount of hemoglobin circulating red cell mass Consequences of anemia - symptoms • ??????????? Dg. of anemia - history • • • • • • • • • • Age of onset Duration of illness Prior therapy of anemia Suddennes or severity of anemia Chronic blood loss Hemolytic episodes Toxic exposures Dietary history Family history, racial background Underlying diseases Anemia – consequences, symptoms • Fatigue, syncope, dyspnea • Impairment of organ function due to hypoxia • Pallor, postural hypotension )decreased blood volume) • Heart murmurs, heart failure . Increased cardiac output Anemia • Not a diagnosis per se • Look for an underlying problem • History, physical examination Anaemia decrease in the total circulating red cell mass (hematocrit, hemoglobin concentration) Classification: A. underlying mechanism blood loss M A increased destruction Y decreased production C B. morphology of erythrocytes O size (micro-, macro-, normocytic) M B shape (spherocytosis, stomato-,...) I N color (degree of hemoglobinization: E normo- hypo-, hyperchromic) Blood loss •acute or chronic •internal or external Acute • Hypovolemia – shock • Anemia – normocytic normochromic • Shift of water – hemodilution –↓ hematocrite • Compensatory increase of red cell production • Reticulocytes • Chronic → loss of iron→ iron deficiency • hypochromic sideropenic anemia Iron deficiency anemia mechanism: blood loss, decreased production body iron = functional + storage F - 2g, M - 6g inadequate intake for metabolic demands Lack in diet or low absorption most common nutritional disorder in the world 2. Increased requirement (children, pregn., lact) !!!3. Chronic blood loss!!! - GIT, GYN most important cause of iron deficiency Hypochromic microcytic sideropenic anemia Small hemoglobinization (narrow Hb rim -periphery) Small red cells Iron deficiency Scattered fully hemoglobinized cells - blood transfusion PB: ery pale + small BM: erythroid hyperplasia, loss of iron alopecia, koilonychia, atrophy of tongue, gastric mucosa Plummer-Vinson (Kelly-Patterson) syndrome: siderop.an., atrophic glossitis, esophageal webs Iron deficiency anaemia Pallor conjunctiva skin pale palmar creases Iron deficiency anaemia koilonychia nails concave (or flat), ridged, brittle Iron deficiency anaemia angular cheilosis fissuring and ulceration; pallor Iron deficiency anaemia flattening and loss of papillae bald, fissured tongue Causes of hypochromic anemia 1. Disorders of iron metabolism 2. Disorders of heme synthesis 3. Disorders of globin synthesis (thalassemia) Ad 1. Iron deficiency • Blood loss • Poor intake - growth, pregnancy, lactation • Malabsorption • Chronic infections or inflammatory states • neoplasia Anaemia decrease in the total circulating red cell mass (hematocrit, hemoglobin concentration) Classification: A. underlying mechanism blood loss → increased destruction decreased production Increased destruction =lysis of red cells=hemolysis • • intravascular – rare - mechanical injury – artificial valves or microthrombi, exogenous toxic agents, complement fixation (transfusion of mismatched blood) extravascular - more common, when red cells considered foreign or less deformable Hemolytic anemia Abnormality: intracorpuscular or extracorpuscular hereditary (intra) or acquired (extra) Hemolytic anemia • premature destruction of red cells • accumulation of the products of the hemoglobin catabolism • BM – increased erythropoiesis, extreme: extramedullary hematopoiesis • PB: reticulocytosis • high bilirubin –gallstones; jaundice, blr in urine • chronic duration: hemosiderosis Main clinical symptoms anemia, splenomegaly, jaundice; gallstones Haemolytic anaemia splenomegaly and jaundice Haemolytic anaemia jaundice normal Increased destruction of ery=hemolysis I. Intrinsic (intracorpuscular) causes A. hereditary • membrane – cytoskeleton, lipid synthesis • enzymes – deficiencies - G6PD, glutathione synthetase, pyruvate kinase • hemoglobin - deficient synthesis of globin, structurally abnormal Hb B. acquired • membrane defect: paroxysmal nocturnal hemoglobinuria • II. Extrinsic (extracorpuscular) causes • antibodies, trauma, infection, chemical injury sequestration Examples of hemolytic anemia • Membrane defects – • Proteins underlying the red cell membrane • Shape, stability, flexibility Hereditary spherocytosis (peripheral smear) anisocytosis and several dark-appearing spherocytes with no central pallor. Howell-Jolly bodies (small dark nuclear remnants) Hereditary spherocytosis AD (AR, sporadic);most common her. hemol. A. Membrane defect – cytoskeleton – protein spectrin (and ankyrin) deficiency Round erythrocyte= spherocyte, less deformable Vulnerable to spleen sequestration and destruction Main clinical symptoms anemia, splenomegaly, jaundice; gallstones Chronic hemolytic anemia (mild to normal) Acute anemic episodes: aplastic crisis (parvovirus) hemolytic crisis Splenic sinus A red cell squeezing from the red pulp cordsinto the sinus lumen. Note the degree of deformability required for red cells to pass through the wall of the sinus. Red cell membrane cytoskeleton Alterations leading to spherocytosis and hemolysis Mutations weakening interactions involving α-spectrin, β-spectrin, ankyrin band 4.2, or band 3 cause the normal biconcave red cell to lose membrane fragments and become spherical spherocytic cells: less deformable than normal, become trapped in the Pathophysiology of hereditary spherocytosis Haemolytic anaemia: reticulocytes precip. RNA Hereditary elliptocytosis Usually mild, rarely severe Hemolytic anemia • Intracorpuscular • Enzyme deficiencies G6PD deficiency enzymes protecting the red cell against the oxidative stress G6PD deficiency → loss of protection → oxidant injury infections, drugs, beans (favism) → hemolysis; otherwise normal morphologic changes of chronic HA rarely present hundreds of genetic forms of G6PD common pathologic alleles: G6PDA-, G6PD Mediterranean X-linked→ males homozygous, women heterozygous Mediterranean, Middle East, Africa Protection against malaria G6PD deficiency • Clinical and laboratory findings • Episode of acute hemolytic anemia in anotherwise healthy person; neonatal jaundice • following oxid. injury – drug (antimal. – primaquine,; sulfoamides, nitrofurantoin, nalidixic acid; TNT, , infections, food • Variable severity Enzyme deficiency: G6PD deficiency effects of oxidant drug exposure (PB) Red cells with precipitates of denatured globin (Heinz bodies) splenic macrophages pluck out these inclusions → "bite cells" Increased destruction of ery=hemolysis I. Intrinsic causes A. hereditary membrane – cytoskeleton, lipid synthesis enzymes – deficiencies - G6PD, glutathione synthetase, pyruvate kinase →hemoglobin – abnormal quantity (deficient synthesis of globin) quality (structurally abnormal Hb) Sickle cell anemia (PB) • • • • • • • Shape: sickle Hereditary hemoglobinopathy Structurally abnormal hemoglobin HbS abnormal physiochemical properties B-globin – 6th position, Molecular defect: point mutation valine for glutamic acid Sickle cell anemia Hemolysis, microvascular occlusion Sickle cell anemia • Oxyg. HbS: liquid • Deoxyg.:viscous gel →fibers HbS - aggregation and polymerization • Sickle shape; Initially: reversible (with oxygenation) • Repeated: irreversible sickling • Membrane damage Rate and degree of sickling 1. Amount of HbS Heterozygotes: HbS and HbA – only sickle cell trait (sickling when marked hypoxia) Homozygotes: severe anemia 2. Hemoglobin concentration the higher, the worse 3. Fall in pH → deoxygenation Sickle cell anemia - clinical manifestation 1. chronic hemolytic anemia (ery survival 20 days) chronic hyperbilirubinemia, Hbemia, jaundice, gallstones aplastic crisis 2. occlusion of small vessels → thrombosis, ischemia, necrosis painful crises 3. splenomegaly 4. increased susceptibility to infections 5. activation of the bone marrow, extramedullary haematopoiesis Diagnosis • • • • Clinical, laboratory – blood smear HbS - electrophoresis Clinical course variable Therapy symptomatic Thalassemia • • • • • Deficient synthesis of globin chains Globin chain absent or amount reduced β - major, minor (more common), intermedia β +,0 Homo/heterozygous • α +,0 Scleral jaundice Haemolytic autoimmune anaemia Pathogenesis of β-thalassemia major aggregates of unpaired α-globin chains not visible Blood transfusions correct the anemia reduce the stimulus for marrow expansion, but add to systemic iron overload Thalassemia major: gallbladder - bilirubin gallstones Immunohemolytic anemia • Antibodies • Coombs test Raynaud phenomenon autoimmnune haemolytic anaemia Erythroblastosis fetalis Decreased production of red cells Deficiency of vital substrates disorders of proliferation and differentiation stem cells erythroblasts Impaired: DNA synthesis – B12, folic acid – megaloblastic hemoglobin synthesis - heme (lack of iron) - globin Others: anemia of chron. dis., AA, PRCA Megaloblastic anemia • impaired DNA synthesis • characteristic morphologic changes blood (macrocytes), bone marrow (megaloblasts) • Deficiency of vit. B12 • Folic acid Megaloblastic anaemia Vitamin B12 absorption Deficiency of vit. B12 1. Decreased intake – diet, vegetarianism 2. Impaired absorption Intrinsic factor deficiency – pernicious anemia, gastrectomy Malabsorption Intestinal dis., resection of ileum Parasitic uptake, bacterial overgrowth 3. Increased requirement pregnancy, hyperthyroidism, disseminated cancer Vit. B12 deficiency • BM and blood, CNS, (pernicious: GIT) • GIT: beefy tongue – atrophic glossitis • CNS – spinal cord - myelin degenaration laterodorsal tracts – balance, motoric, sensitive • Pernicious: stomach: chronic gastritis, intestinal metaplasia, higher risk of carcinoma Pernicious anemia • Older people • Autoimmune Ab • Poss. with autoimmune thyroiditis, adrenalitis Megaloblastic anaemia Acute leukaemia Diffferential diagnosis Megaloblastic anaemia hypersegmented neutrophils (macropolycyte) Megaloblastic anaemia pernicious lemon-yellow appearance pallor (anaemia) + jaundice (ineffective erythropoiesis) Pernicious anaemia (38 ys.) premature greying, blue eyes, vitiligo Beefy tongue atrophic glossitis (Hunter) vit. B12 deficiency Pernicious anaemia Dorsolateral spinal cord demyelination Folate deficiency • Decreased intake • Increased requirements • Impaired use • Relative deficiency • Megaloblastic anemia; no neurological symptoms • Cheilosis, glossitis, dermatitis Anemia of chronic disease *Infections *immunologic *neoplasms Mechanism: defect in reutilization of iron (transfer, cytokines) ! abundant storage iron Anemia: normo, normo or hypo, micro Aplastic anemia • Failure or suppression of myeloid stem cell • PANCYTOPENIA • primary OR secondary - drugs , chemicals infections irradiation inherited – Fanconi Or cause unknown… BM: hypocellular, PB: pancytopenia, symptoms spleen normal Special subgroup: pure red cell anemia Aplastic anemia Markedly hypocellular marrow contains mainly fat cells.