Glycogen Formation
advertisement
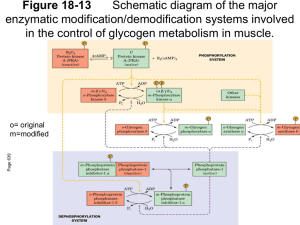
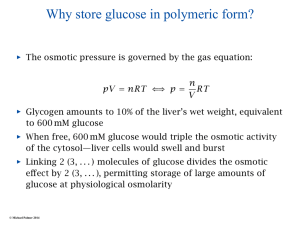
Glycogen Metabolism Variation of liver glycogen levels between meals and during the nocturnal fast. In muscle the final products of glycogen breakdown depend on the type of muscle fiber. Red muscle fibers - many mitochondria and much myoglobin. - Glucose is converted primarily to pyruvate that can be completely oxidized to CO2 and water. White muscle fibers - few mitochondria and little myoglobin - break down glucose primarily to lactate - can do this very rapidly. chicken breast - white muscle fibers -capable of high energy output for short periods chicken heart - red muscle fibers capable of sustained activity but stores glycogen for periods of increased demand Duck breast Turkey breast Most skeletal muscles of humans are a mixture of red and white fibers. Structure of Glycogen - one branch point about every ten sugars - glycogen granules present in cytosol - granules about 10-40 nm in diameter - ~100,000 glucose units in a granule Glycogen Biosynthesis - takes place in the cytosol - utilizes an activated form of glucose - UDP-glucose - UDP-glucose is made from Glucose-1-phosphate and UTP The phosphoglucomutase reaction. UDP-Glucose Pyrophosphorylase Glycogen Synthesis is Initiated on Glycogenin -the first step in glycogen synthesis is the transfer of a glucose unit from UDP-glucose to a tyrosine in glycogenin. - glycogenin autocatalytically extends the glucan chain ~7 Glc units, then glycogen synthase takes over, along with glycogen branching enzyme. Enzymes of Glycogen Metabolism Form a Complex with the Glycogen Particle GN - glycogenin GS - glycogen synthase GP - glycogen phosphorylase PhK - phosphorylase kinase RG1 - phosphatase reg. subunit CS1 - phosphatase catal. subunit Glycogen Branching Enzyme - transfers a ~7 glucose segment Glycogen breakdown Dietary: Involves a amylase Creates limit dextrins and maltose Debranching Hydrolysis produces 2 glucose from one maltose Metabolic-intracellular Involves glycogen phosphorylase Debranching Produces Glucose-1-phosphate Phosphoglucomutase converts Gluc-1-phosphate to Gluc-6-phosphate Dietary breakdown of Starch Figure 22.11 (a) The sites of hydrolysis of starch by α- and βamylases are indicated. a-amylase (saliva and pancreas) b-amylase (in plants) a-amylase can cleave to maltose and maltotriose (2 glucose and 3 glucose moieties) but stops within 4 glucoses of a branch, so leave “limit dextrins” that need debranching. Dietary carbohydrate breakdown Figure 22.12 The reactions of debranching enzyme. Transfer of a group of three glucose residues from a limit branch to another branch is followed by cleavage of the bond linking the remaining residue at the branch. Glycogenolysis Intracellular - glycogen breakdown is not simply a reversal of biosynthesis - different reactions are involved. Glycogen phosphorylase cleaves glucose residues off the non-reducing ends of the chains by addition of inorganic phosphate (phosphorolysis). - the enzyme only removes glucose units that are 4 or more residues from a branch point. Glycogen Debranching Enzyme The enzyme has 2 different activities: 1. oligo-(a-1,4a-1,4)glucantransferase 2. 2. amylo-a-(1,6)-glucosidase Glycogen phosphorylase and debranching enzyme give a mixture containing ~10 times as much G1P as glucose. Why phosphorolysis? - product is already phosphorylated - no need to use an ATP - G1P can be readily converted into G6P by phosphoglucomutase. Phosphorylase Kinase is activated Phosphorylation and by Calcium Ions Phosphorylase kinase is activated by phosphorylation by an enzyme called protein kinase A (PKA). Muscle contraction Hormone-triggered cyclic AMP release Ca2+ release Ca2+ -free kinase inactive Ca2+ kinase partly active Phosphorylated kinase fully active by Muscle contraction Hormone-triggered cyclic AMP release Ca2+ release Ca2+ -free kinase inactive Ca2+ kinase partly active Phosphorylated kinase fully active Hormonal Control of Glycogen Metabolism Insulin, glucagon, and epinephrine profoundly influence glycogen metabolism. Glucagon and epinephrine release triggers the breakdown of glycogen. Glucagon and epinephrine bind to receptors on the plasma membrane of cells and trigger the release of the “second messenger” cyclic AMP. Formation of Cyclic AMP Cyclic AMP activation of protein kinase A Cyclic AMP-dependent protein kinase A (PKA) is activated when the two regulatory subunits bind cAMP and then release the active catalytic subunits. Activation of Phosphorylase Protein Phosphatase 1 (PP1) Reverses the effects of the kinases and plays an important role in regulating glycogen metabolism. It increases the rate of glycogen synthesis and decreases the rate of glycogen breakdown. Inactivation of Glycogen Synthase Epinephrine enhances glycogen breakdown while decreasing synthesis Blood Glucose Levels are Regulated by Glycogen metabolism in the Liver The liver maintains the concentration of glucose in the blood between 80 and 120 mg/100 ml. The glucose sensor in the liver is phosphorylase a. - when glucose binds it exposes the phosphate group to protein phosphatase 1. - although PP1is normally bound to phosphorylase a it only cleaves off the Pi group when phosphorylase a binds glucose. - PP1 is released from phosphorylase b and then begins to dephosphorylate glycogen synthase (activates it). The infusion of glucose into the bloodstream leads to the inactivation of phosphorylase, followed by the activation of glycogen synthase in the liver. Insulin Stimulates Glycogen Synthesis by Activating Protein Phosphatase 1 The insulin-sensitive protein kinase phosphorylates the G subunit of PP1 at a different site than PKA, making it more active. The activated PP1 then dephosphorylates glycogen synthase, phosphorylase kinase, and phosphorylase causing increased glycogen synthesis and decreased glycogen breakdown. Different Effects of Glucagon and Epinephrine Epinephrine - “fight or flight” hormone Also known as Adrenaline - rate of glycolysis may increase 2000-fold Epinephrine activates glycogen breakdown in both muscle and liver. Glucagon has a different role, maintaining blood glucose levels. Glucagon does not activate glycogen breakdown in muscle. Consumption of muscle glycogen during exercise. Rate of glycogen replenishment after exhaustive exercice. von Gierke Disease - A Glycogen Storage Disease - enlarged abdomen, thin extremities, striking elevation of serum triglycerides, hypoglycemia, etc. - massive accumulation of glycogen in liver and kidneys. - in 1952 Carl and Gerti Cori showed that it results from the absence of glucose-6-phosphatase, which blocks the last steps of glycogenolysis and gluconeogenesis. - greatly increased glycolysis resulting in lactic acidosis. - treatment attempts to maintain blood glucose levels.