Chapter 8
advertisement
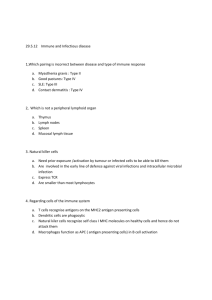
Chapter 8 The Immune System The immune system • Two general classifications 1. Non-specific immune system 2. Specific immune system Visit the Immune System at www.niaid.nih.gov/final/immun/immun.htm Cells of the immune system The components of non-specific immunity • External mechanisms – – – – Skin Digestive tract Respiratory tract Urinary tract • Internal mechanisms – – – – Visit The Anatomy of the Immune System at www-micro.msb.le.ac.uk/MBchB/2b.html Phagocytic cells NK cells Complement proteins Interferons Phagocytosis • • Process by which unwanted particles are engulfed and destroyed by digestive enzymes Two major groups of cells are involved: 1. Neutrophils 2. Mononuclear phagocytes, which include: • • • Monocytes Macrophages Tissue-specific phagocytes Phagocytosis by a neutrophil or macrophage Natural killer (NK) cells • Non-T and non-B lymphocytes thought to be involved with immune surveillance against cancer • Method by which NK cells destroy virally infected and tumor cells is unknown Complement proteins • System has nine protein components (C1 through C9) • Exist in inactive state in blood and other fluids • Destroy cells that have been marked for elimination by antibodies • Activation of the system occurs when antibodies bind with antigens on the invading cells • Series of events follow that results in water entering the cells and causing them to burst Interferons • Polypeptides that interfere with ability of viruses to replicate • Produced by cells infected with viruses; act on neighboring cells to prevent infection • Mechanics of the action are – Direct: produces cellular enzymes that prevent viral protein synthesis and destruction of viral messenger RNA – Indirect: stimulates NK and killer T cell activity and antibody production in plasma cells The two classifications of the specific immune mechanisms 1. Humoral 2. Cell-mediated Specific immune mechanisms • • Target antigen molecules Antigen molecules exhibit two characteristics 1. They stimulate antibody production 2. They combine with the specific antibody The four components of humoral immunity 1. 2. 3. 4. B cells Plasma cells Antibodies Memory B cells The components of cell-mediated immunity • T cells, which give rise to: – Killer T cells – Helper T cells – Suppressor T cells – Memory T cells B Cells – Respond to antigens presented by macrophages – After exposure, divide into • Plasma cells—secrete antibodies specific to the antigen • Memory B cells—remember a previous invader and eliminate them Role of B cells in humoral immunity Antibodies • Glycoproteins produced and secreted by plasma cells • Antibody itself does not directly destroy cells but activates nonspecific immune mechanisms For more information, visit Antibody Production at www.cellsalive.com/antibody.htm The T cells • Killer T cells – Must be near or in contact with the cell targeted for destruction – Produce lymphotoxins – Release interferons and substances that enhance phagocytosis • Helper T cells – Stimulate cytotoxic action of killer T cells – Increase antibody production by plasma cells The T cells (cont.) • Suppressor T cells – Regulate action of killer T cells and development of B cells into plasma cells – Keep immune defense from exceeding limits necessary to destroy invading organism • Memory T cells – Recognize an antigen from previous exposure Role of T cells in cellular immunity Exercise alters several components of the immune function, including • Exercise results in leukocytosis • Exercise results in lymphocytosis • Exercise may increase interferon levels, but the significance is unknown HIV positive individuals and exercise • Exercise does not exacerbate the progression of HIV and may slow it. • Exercise can help HIV-infected individuals maintain health. • Moderate aerobic exercise can increase helper T cell and NK cell counts. • Resistance training can help to maintain or increase muscle mass and so diminish the weight loss characteristic of stages 2 and 3 of HIV infection. For more information, visit Comprehensive AIDS and HIV Information www.thebody.com How to minimize the risk of becoming ill 1. Allow sufficient time between training sessions for recovery. 2. Avoid extremely long training sessions 3. Use periodization of training 4. Avoid training monotony by ensuring variation in training load 5. When increasing the training load, do so on hard days. Don’t eliminate recovery days 6. When recovering from overtraining or illness, begin with light training and increase gradually. 7. Monitor and record mood, feelings of fatigue, and muscle soreness; decrease the training load if the session seems harder than usual. How to minimize the risk of illness (cont.) 8. 9. 10. 11. Keep other stresses to a minimum. Get regular and adequate sleep Get more rest after travel across time zones Pay attention to diet and make sure it is wellbalanced 12. Ensure adequate total dietary intake 13. Consider drinking carbohydrate sports drinks before, during and after prolonged workouts 14. Consider vaccination. Guidelines for training and competition during an infection – Exercise tolerance may be reduced during infection – Exercising with an infection may increase the duration of the illness – Iron supplements should be avoided to limit bacterial infection – Training should be stopped if fever or systemic symptoms are present – Training should be resumed gradually – Team members with infection should be isolated as much as possible from the rest of the team