Approach to the Cyanotic Infant
advertisement
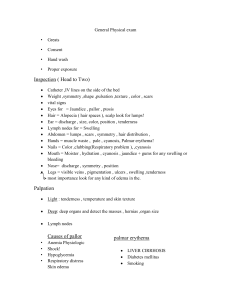
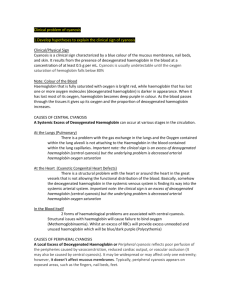
Approach to the Cyanotic Infant Billie Parsley Goals Recognition of a cyanotic infant What to do in any setting from ICU to rural community pediatric practice What questions to ask What to look for What imaging to order What test to order Case 39 week male born at home in uncomplicated vaginal delivery Presented at ACH ED 24 hours old due to temp of 35.1 rectal Sats in 50s, HR 100, RR 80, BP 76/59 Cyanotic on general appearance What is cyanosis? Cyanosis is a bluish discoloration of the tissue that results when the absolute level of reduced hemoglobin (when not combined with oxygen) in the capillary bed exceeds 3 g/dL. The appearance of cyanosis depends upon the total amount of reduced hemoglobin rather than the ratio of reduced to oxygenated hemoglobin. Cyanosis Two mechanisms result in cyanosis: Peripheral cyanosis Normal systemic arterial oxygen saturation and increased tissue oxygen extraction that leads to a widened systemic arteriovenous oxygen difference of >60% (normal 40%) resulting in an increased concentration of reduced hemoglobin on the venous side of the capillary bed. Central cyanosis caused by systemic arterial oxygen desaturation Don’t confuse central cyanosis with acrocyanosis!!!! Acrocyanosis-common physical finding in newborns as a result of peripheral vasoconstriction Cyanosis Best indicator is the tongue-due to free of pigmentation and has rich vascular supply. Also seen in lips, nails, earlobes, mucous membranes Cyanosis Depends on multiple factors Hemoglobin Fetal hemoglobin Skin Pigment Factors affecting the hemoglobin dissociation curve Cause Alveolar hypoventilation Nml response is hypercarbia but can also cause hypoxemia Ventilation Perfusion mismatch Nml is for areas with decreased ventilation to have decreased blood flow, but alterations in this cause hypoxemia Diffusion Impairment Oxygen molecules must diffuse from alveoli to pulmonary capillary to oxygenate hemoglobin Right to Left Shunt Systemic venous blood bypasses ventilated alveoli and returns to the left heart without being oxygenated Disturbed Hemoglobin Decreased oxygen affinity History Pregnancy Maternal Diabetes-associated with cyanotic heart dz. Polyhydramnios-associated with fetal airway, esophageal, neurologic abnormalities Oligohydramnios-associated with renal defects and pulmonary hypoplasia Drug Use during pregnancy Maternal Serology US results Previous complications with pregnancy (stillborn/multiple spontaneous abortions) Medication Use during pregnancy History Perinatal/Peripartum Gestational Age Prolonged/Premature Rupture of Membranes What/How treatment given for illness during pregnancy (GBS) Maternal fever Birth Trauma Neonatal polycythemia Hypoglycemia Meconium Staining-associated with Meconium Aspiration syndrome and P-HTN Hospital course post delivery History HPI Fever Exposure Trauma Well water Seizure Poor Feeding Decreased urine output Medications Different Temperatures between extremities Cough/Congestion Rashes Changes in skin “birth marks” Abnormal breathing-pauses in breathing Weight loss or gain Edema History Diet What (could mom be taking in meds that get into breastmilk) How long does it take? Perspiration with feeds Coughing/Gagging/Gurgling with feeds Medications Family History Hemoglobinopathies Congenital Cardiac Abnormalities Cystic Fibrosis Neuromusclar Disorders Physical Exam *The presence and degree of respiratory distress are very important factors in differentiating your 2 main causes of Cyanosis-Cardiac vs. Respiratory General exam: Comfort, WOB, LOC, Color, Head: Fontanel, Shape of Head, eccymosis, lacerations, Pupils, nose shape and location, shape of chin and size, mouth size, moisture, cleft palate, Neck: size of vessels, abnormal masses Abdomen: HSM, ascities, Skin: Rashes, birthmarks , mottled, slate gray color associated with methemolglobinemia Limb abnormalities Physical Exam Respiratory Exam Respiratory Rate (newborn nml 40-60) Low RR-alveolar hypoventilation Tachypnea-Cardiac or Pulmonary cause Regularity of RR apnea events Grunting (prevents end expiratory alveolar collapse) Nasal flare (reduces nasal resistance) Stridor Tracheal Deviation Chest wall movement Retractions Accessory muscle use Auscultation Physical Exam Cardiac Exam-not as severe respiratory distress Heart Rate Pulses Perfusion Auscultation Four Extremity Blood Pressure Pre/Post Ductal oxygen Saturation Point of Maximal Impulse Labs ABG-for arterial oxygenation Painful and can cause increasing agitation Methemoglobinemia oxygen saturation will be low but measured PO2 will be normal Elevated arterial PCO2 suggest pulmonary cause Metabolic acidosis indicates poor perfusion-possible due to poor cardiac output or oxygen delivery or shock. CBC Can show high hgb/hct in polycythemia I/T ratio Blood glucose Blood Culture Imaging Trauma Airway Situs of heart, stomach, liver-any abnormalities in location point towards cardiac disease Heart size and shape Lung fields Vascular Markings Decreased vascular markings can be seen in cyanotic cardiac lesions and pulmonary hypertension Other Test Hyperoxia testing—Right radial artery PaO2 (preductal) measured on RA and after 10 minutes on 100%FiO2 if right radial arterial PaO2 on 100% FiO2 is less than 150mmHg, severe congenital heart disease is likely. The infant is presumed to have ductal dependant congenital heart disease and the low PaO2 is attributed to the obligatory mixing of oxygenated with deoxygenated blood within the circulatory system. Other Test Echo Transposition Tetralogy of Fallot Truncus arteriosus Total anomalous pulmonary venous Return Tricuspid “Tons” of others EKG Managment ABCs Access-venous and arterial if possible Ventilation as needed Cautious fluid resuscitation Antibiotics Prostaglandin Infusion Prostaglandin Goal is to prevent closure of the PDA if this is where mixing is occurring. Improvement normally seen within 1-2 hours Side effects: APNEA and peripheral vasodilatation with hypotension Case Review Mom GBS + treated with oral clindamycin Baby with severe Pulmonary HTN with near systemic pressures By 48 hours of life on ECMO on way to Edmonton