Biological Safety
advertisement
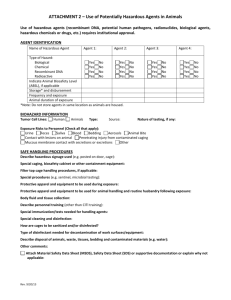
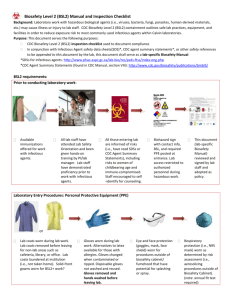
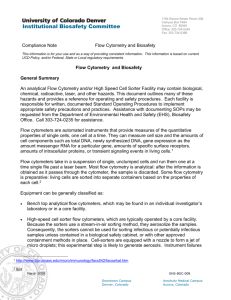
OVERVIEW OF INDUSTRIAL HYGIENE UNIVERSITY OF HOUSTON – DOWNTOWN CAMPUS BIOLOGICAL SAFETY Discipline of Biosafety grew out of research involving biological warfare agents at Fort Detrick in Frederick, MD. The Chemical Warfare Service was established by the US Army in 1941 and the National Academy of Science formed a biological warfare committee in 1942. Microbiologists from ASM served as advisors. Fort Detrick Biological Defense Research Program formed the framework for the discipline of biosafety. BIOLOGICAL SAFETY The responsibility of the biosafety professional, infection control practitioner, or hospital epidemiologist again shifts to include the task of assessing the need for appropriate containment for patients. OSHA Bloodborne Pathogens (1991) developed as a result of HIV in the 1980s, Hepatitis B infection, etc.. The biosafety professional uses similar practices to define and control workplace hazards re IH. HAZARD IDENTIFICATION Microorganisms are a diverse group of microscopic organisms that includes bacteria, fungi, algae, protozoa, viruses, and prions. Pathogenic or disease-producing are a small portion of total microbials. Also, fungi produce spores and mycotoxins. Other biological agents such as pollen, mites, urine proteins, animal dander, and snake venoms broaden the scope of biological hazards to consider. MICROORGANISMS - Prokaryotes – organisms in which DNA is not physically separated from the cytoplasm; small size (around 1 um in diameter) and absence of a nuclear membrane. - Eukaryotes – organisms containing a membrane-bound nucleus; larger and contain a membrane-bound nucleus and organelles such as mitochondria. - Four major groups of eukaryotes are algae, protozoa, fungi, and slime molds. - Viruses – totally dependent on hosts for replication; smallest infectious agents. - Viroids and Prions INFECTION Infection is a general term applied to the entry and development of multiplication of an infectious agent. Further defined as an invasion of the body by pathogenic microorganisms and the reaction of the tissues to their presence and to the toxins generated. Normal flora can take advantage of a lowering of host immunity to produce an infectious disease. Infectious disease is not always the end result of exposure to and colonization by an infectious agent; depends on the virulence of the agent, the route of infection, and the relative immunity and health of the host. EPIDEMIOLOGY Potential for work-associated infection. Epidemiology methods provide the tools to evaluate the extent and nature of worker exposure. Defining the event or illness/infection, determining the population at risk, establishing the factors affecting exposure, and developing intervention controls are all part of the process to prevent occurrence or recurrence of infections. Sulkin and Pike; 4K+ infections with 168 deaths. 10 most frequently reported agents or diseases for lab-acquired infections: brucellosis, Q fever, hepatitis, typhold fever, tularemia, TB, etc.; routes – percutaneous inoculation; aerosol inhalation; mucous membrane contact; ingestion. WORKPLACES - Agricultural environments and processing facilities; - Microbiology, public health, clinical labs; - Hospital and Health Care facilities; - Biotechnology facilities; - Animal facilities and veterinary practices; and, - Miscellaneous. RISK ASSESSMENT Modes of Transmission Routes of Entry Infectious Dose Agent Viability and Virulence Host Susceptibility Other Factors BIOSAFETY CONTAINMENT - CDC/NIH Guidelines for Microbiological and Biomedical Laboratories. Risk management is achieved through use of practices, facilities, and equipment specified in defined biosafety containment levels. Biosafety practices are an important part of a program to manage the risk of exposure to potentially infectious agents. - NIH Guidelines for Research involving Recombinant DNA Molecules. BIOSAFETY CONTAINMENT LEVELS - Biosafety Level 1 (BSL-1) – work with defined and well-characterized strains of viable microorganisms of no known or of minimal potential hazard to lab personnel or the environment. - Biosafety Level 2 (BSL-2) – work with many moderate-risk agents present in the community (indigenous) and associated with human disease of varying degrees of severity. e.g. clinical, diagnostic, teaching, and other research facilities with individual level of competency BIOSAFETY CONTAINMENT LEVELS - Biosafety Level 3 (BSL-3) – work with indigenous or exotic agents where the potential for infection by aerosols is real and the disease may have serious or lethal consequences. e.g. clinical diagnostic microbiology work when TB or brucellosis is suspected, etc. - Biosafety Level 4 (BSL-4) – work with dangerous and exotic agents that pose a high individual risk of life-threatening disease. Agents have a low infectious dose and poses a danger for the community from person-to-person spread. e.g. stringent requirements such as a Class III BSC, etc. HAZARD CONTROL Containment Facility Design Safety Equipment BSCs (Class I, II, III) Work Practices Decontamination BIOSAFETY PROGRAM MANAGEMENT Program Support Biosafety Specialist Institutional Biosafety Committee Biosafety Manual Occupational Health Program Information and Education TOPICS IN BIOSAFETY Bloodborne Pathogens Hepatitis B and C Viruses HIV Tuberculosis Bioterrorism Legionellosis Occupational Health Program BRI vs. SBS