Diabetes - Health and Social Care
advertisement

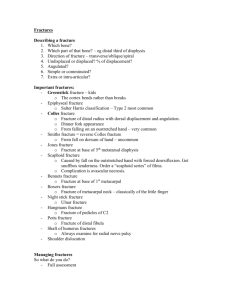
Unit MPII 002 Managing paediatric illness and injury (Part 1) MPII 002 Managing paediatric illness and injury 1 credit This part of the unit looks at first aid for infants and children: • • • • with a suspected fracture and a dislocation with a head, a neck and a back injury with conditions affecting the eyes, ears and nose with a chronic medical condition or sudden illness. Connector What is the difference between fracture and a dislocation? Be prepared to give feedback! Research activity Each group to research the following type of fracture: Group A: Greenstick fracture Group B: Open fracture Group C: Closed fracture Group D: Hairline fracture Common types of fractures 1.1 • Greenstick fracture: the bone bends and splits but does not break (just like a green stick). There is little damage to the surrounding tissue. • Open fracture: the broken end of the bone breaks through the skin and may stick out. • Closed fracture: the bone is broken but does not damage the skin. • Hairline fracture: the bone is only partially fractured. These fractures can be difficult to detect on x-rays. How to manage a fracture 1.2 • Do not attempt to straighten a broken limb. • Do not give anything to eat or drink Leg injury Keep the injured limb supported. Make a splint Arm and collarbone Immobilise the affected area Fracture Signs of shock Lie the child down. Raise their legs above the level of their heart. Make sure you keep the child warm Treat wound Control the bleeding and loosely cover the wound with a dressing How to manage a dislocation 1.3 & 1.4 • The principles of managing a dislocation are the same as for managing a fracture. • Get the child to hospital, immobilise and support the affected area. Head injuries 2.1 Dazed and confused ? Dizziness and nausea ? Concussion Brief loss of consciousness Severe headache ? Skull fracture ? Blow to the head Bruise or wound on head Cerebral compression High temperature and flushed face ? ? ? ? ? ? ? What are the missing signs and symptoms? Managing a head injury 2.1 If conscious If unconscious Help to lie down – do not turn head Open airway and check for breathing Control any bleeding from scalp Be prepared to give chest compressions and rescue breaths Dial 999 for ambulance Dial 999 for ambulance If there is discharge from ear, cover Monitor and record vital signs until with sterile dressing help arrives Monitor and record vital signs until help arrives In case of spinal injury, make sure child does not move. Medical staff will confirm or rule out spinal injury. Foreign bodies in eyes, ears and nose 3.1 Eyes Ears • Try to remove with swab • Try flushing out • If metal or glass, take to hospital immediately • If an insect, try flushing out • Do not remove if object is hard, take to hospital Nose • Do not try to remove • Take to hospital immediately Other common eye injuries 3.2 Injuries Signs and symptoms Treatment Chemical burn • Red, watering eye • Pain and difficulty in opening eye • Wash chemical out immediately • Cover injured eye • Call 999 for ambulance or take to hospital Black eye • Bruising of skin around eye bones • Place an eye pack over eye • Consult doctor if there appears to be serious damage Chronic medical conditions 4.1 Condition Signs and symptoms Treatment Sickle cell anaemia • Suddenly becomes unwell • Severe abdominal/chest pain • Headache/neck stiffness • Contact parents/carers – urgent hospital treatment needed Diabetes – a hypoglycaemic attack (hypo) • Weakness or hunger • Confused/aggressive behaviour • Loss of concentration/ coordination • Rapid shallow breathing • Sweating, dizziness, glazed eyes, headache, trembling or shakiness • Stay with child • Sit them down and reassure • Give sugary drinks and sweet food • If no quick recovery, call ambulance and place child in recovery position Asthma • Shortness of breath • Wheezing • Feeling of tightness in the chest • Make child comfortable and encourage slow breathing • Do not let child lie down • Help child to use their inhaler Meningitis 4.2 Babies under 12 months • Bulging fontanelle. • High temperature. • Floppy or stiff body. • Blotchy pale skin. • High-pitched moaning cry. • Red/purple spots that do not fade under pressure (glass test). • Difficult to wake up. • Refuses to feed. • • • • Older children Neck stiffness and joint pains. Neck arching backwards. Cannot tolerate light. Red/purple spots that do not fade under pressure. Get medical help quickly Febrile convulsions (1) 4.2 Signs and symptoms • Child may be flushed and sweaty and forehead will feel very hot to the touch. • Child may stiffen their limbs which will twitch or shake; this can go on for up to five minutes. • Child may arch their back and clench their fists . • Child may hold their breath, making their face look blue. • Child may be incontinent of urine or faeces. • Child may become unconscious from the violence of the twitching. Febrile convulsions (2) Treatment • Remove any clothing and open the window. • Lay the child down on his/her side. Provide support with a cushion or rolled-up blanket. • Ask a colleague to call for a doctor at once. Call an ambulance if the convulsion lasts for longer than five minutes. • Use tepid water to sponge over the child. The convulsion will stop once the child has cooled down. • Contact the child’s parents or carers to let them know what has happened. • Once recovered, encourage the child to drink plenty of water and give the recommended dose of paracetamolbased syrup. This will help to reduce body temperature and relieve discomfort. Worksheet 1 Work with person sitting beside you and complete worksheet 1. Be Prepared to give feedback! Review Ask the person beside you…