Osteoarthritis
advertisement
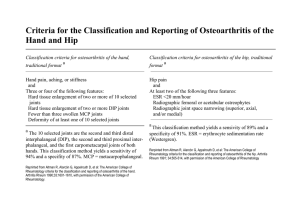
Osteoarthritis and Related Conditions Brian J. Keroack, MD Clinical Features of Osteoarthritis Onset as young as mid 30’s (usually>40) Early OA (1-2 years): Inflammatory symptoms prominent: Morning stiffness (<1hr). “If I just keep going I’m OK.” Red, prominent PIP, DIP joints Normal Radiographs Later: AM stiffness <30 min. ‘Mechanical’ symptoms: Worse with use. “I really pay for what I do.” “I just don’t have the strength I use to.” (e.g. jars, doors) Joint abnormalities preclude normal use Clinical Features of Late OA: continued Little Evidence of Inflammation Deformities more prominent (angulation, bony proliferation) Radiographs abnormal Some patients actually get LESS symptomatic in non-weight bearing joints. You will see many patients with hand deformities that are asymptomatic “My hands really don’t bother me like the use to.” “Once they deformed, they stopped hurting.” Weight bearing joint symptoms usually progress. Risk Factors for Osteoarthritis Weight Trauma Genetics?—Amino acid substitutions in Type II Collagen. Secondary Osteoarthritis (later) Consequences of OA: Spinal Stenosis Erosive Osteoarthritis More aggressive Destructive Persistent symptoms Inflammatory findings on exam Secondary Osteoarthritis Trauma Congenital deformity Endocrinopathies Neuropathic Arthropathy Avascular Necrosis Padget’s Disease Diffuse Idiopathic Skeletal Hyperostosis (DISH) Hemophilia Crystals (CPPD, Hydroxyapetite) Illnesses Associated with Neuropathic Arthropathy (Charcot Joint) Diabetes Alcoholism Tabes Dorsalis Syrinx (meningomyelocele—cord compression) Therapy Joint Conservation Exercise Weight Loss (Wt Bearing Joints) NSAIDS (Cough medicine analogy: not disease modifying) Not benign: Ulcers 4%, greater with risk factors (age>60, coumadin, past ulcer, prednisone use). Hypertension, ACE+Diuretic+NSAID=trouble (e.g. CHF, Renal failure) COX-2: Safer for those at risk for ulcer (>65, coumadin, prednisone, previous ulcer) similar renal effects. Cardiovascular effects? 2.5 X increase in MI or CVA. Mechanisms—1. Increase Thromboxane A2 (platelets stickier).---2. Vascular remodeling (18 months)-Hypertension Therapy: Continued ??DMARDS—not yet The problem: Sclerosis of subchondral bone in mid thirties, apoptosis of chondrocytes in late thirties If DMARDS are to succeed they will have to be studied a decade before symptoms start Remind me not to volunteer for a medicine that might work that I will have for take for 10 years without knowing the long term effects Joint Replacement/Fusion Medical vs Surgical Disease? Bone on Bone (X-rays never told me about symptoms) Night Pain “As soon as I step on the knee it hurts and it is all down hill from there.”