Peer Review & Risk Management Presentation
advertisement

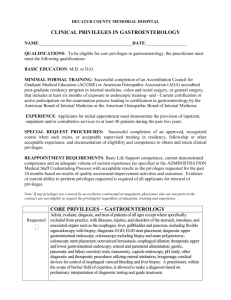
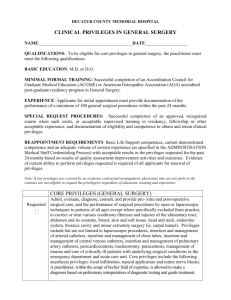
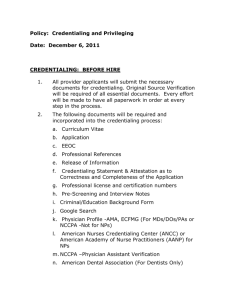
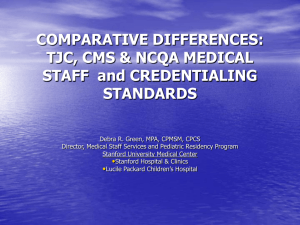
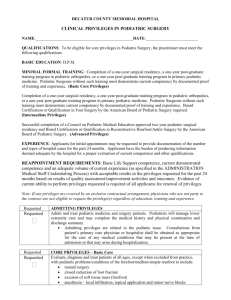
Kentucky Primary Care Association Annual Conference October 19, 2010 Tricia A. Shackelford, Attorney-at-Law Crown Medical Management Group, LLC The process by which a facility and its medical staff reviews a physician's qualifications (or “credentials”) to confirm eligibility for medical staff membership and clinical privileges. The process by which medical practitioners review professional performance of other health care professionals. Necessary qualifications for medical staff membership Procedure for granting and withdrawing staff privileges Mechanism for physician appeals from decisions made regarding staff membership and privileges Six General Areas of Competencies Patient care Medical clinical knowledge Practice-based learning and improvement Interpersonal communication skills Professionalism Systems-based practice Focused Professional Practice Evaluation Continuous evaluation of practitioner performance Challenges to the applicant’s professional license or a voluntary relinquishment of a license; Voluntary or involuntary termination of medical staff membership or reduction of clinical privileges at another facility; Evidence of an unusual pattern or an excessive number of professional liability actions result in a final judgment against the applicant; Documentation as to health status; and Relevant practitioner-specific data, and morbidity and mortality data, when available. Members of the medical staff must apply for reappointment and renewal of clinical privileges every two years Peer evaluations of performance Assessment of professional performance, judgment, interpersonal communication skills, and clinical or technical skills Review of demonstrated current competence Appeal of adverse medical staff determinations Reasons for denial, revocation, reduction, suspension Fair hearing and appeal procedures Process may differ for initial applicants versus existing members of the medical staff “Pure Economic Credentialing” and “Hybrid Economic Credentialing” Malpractice experience Number of hospital admissions Admission diagnoses Average length of stays Inpatient resource utilizations Number of diagnostic tests ordered Outpatient service utilization Ancillary services ordered Payor mix Credentialing and Peer Review Facilities have an independent duty to oversee the care provided to patients in accordance with applicable standards and the facilities bylaws (Darling v. Charleston Cmty. Mem’l Hosp. (Ill. 1965) Because most medical staff members enjoy substantial autonomy over patient care, injured patients have traditionally been limited to seeking recovery from physicians for malpractice. Recognition of Medical Staff Membership as a Property Right Under Kentucky law, membership in a facility’s medical staff creates a property right Facilities must act in accordance with their bylaws and governing policies and cannot apply them in a manner that is unreasonable, arbitrary, or capricious Medical Staff Bylaws as a Contract Denial of Due Process Antitrust Considerations Granting and revoking medical staff privileges Credentialing non-physicians Release of Peer Review Documents Non-Disclosure of Peer Review Documents Releases and Waivers in Applications and Bylaws Kentucky Statutory Immunity Kentucky Case Law Patient Safety and Quality Improvement Act Purposes of HCQIA Peer Review Immunity Scope and Limitations Persons and Entities Qualifying for Immunity Due Process Standard for Professional Review Actions Peer Review Information Required to be Reported National Practitioner Data Bank and Querying Requirements Reporting Information to the NPDB Requesting Information from the NPDB Confidentiality of NPDB Information Reportable Final Adverse Actions Reporting Requirements Eligible Entities Time Limits Subjects of Reports Penalties for Failure to Report Querying HIPDB Correction of Erroneous Information Creation of the Provider/Patient Relationship Implied contract Person seeks treatment Provider accepts the person as a patient Providers have no obligation to accept a person as a patient Exceptions – third party payor contracts, provisions in medical staff bylaws, anti-discrimination restrictions for large providers, on-call physicians and ED patients Effect of the Provider/Patient Relationship Provider is under a duty to provide services to the patient until treatment is no longer needed Patient terminates Provider terminates Appropriate notice Sufficient time to secure substitute care Duty of Facilities to Accept Patients Emergency Treatment (EMTALA, JCAHO, AOA, Tax Code) Non-Emergency Treatment Third-party payor contracts Medicare/Medicaid Hill-Burton Act State Property Tax Exemptions/Charity Care No right is held more sacred, or is more carefully guarded by the common law, than the right of every individual to the possession and control of his own person, free from all restraint or interference from others, unless by clear and unquestionable authority of law (Union Pac. R.R. Co. v. Botsford (1891)). Valid informed consent requires disclosure to the patient of The patient’s condition; The nature of the proposed treatment; The benefits reasonably expected from a proposed treatment, together with the material risks and dangers of the proposed treatment; and Treatment alternatives, as well as the risks and the benefits of such alternatives. Additional procedures are necessary to accomplish the initial treatment for which there was consent; Emergency circumstances where a presumption can be made that the patient would consent to protect the patient’s life; or Giving the patient all the relevant information would be harmful to the patient Reasons for incompetence Youth Mental Incompetence Illness Injury External Influences (Drugs/Alcohol) Liability for Corporate Negligence Negligent Credentialing/Peer Review Inadequate Facilities/Equipment/Supplies Promulgation and Enforcement of Policies and Procedures Liability for Acts of Employees Intentional Acts Negligent Acts Duty Breach Causation Liability for Acts of Physicians Discovery Rule Wrongful Death Tolling the Statute of Limitations Claims Made v. Occurrence Based Tail Coverage Corporate Coverage v. Individual Coverage Obtain informed consent Document care and treatment thoroughly contemporaneous with the services provided Assist patient with an untoward outcome Contact risk management, your insurance carrier, and your attorney immediately Be contrite but never admit a mistake Tricia A. Shackelford, Attorney-at-Law Crown Medical Management Group, LLC 3288 Eagle View Lane, Suite 300 Lexington, Kentucky 40509 (859) 264-2668 – office (859) 264-2661 - facsimile tshackelford@crownmmg.com

![[Medical Staff] Lifecycle of a [hospital employed] physician](http://s2.studylib.net/store/data/005745453_1-fdfe00678075ff3b71119f872900f226-300x300.png)