Laura Knecht, MD - Barrow Hypothalamic Hamartoma Blog
advertisement
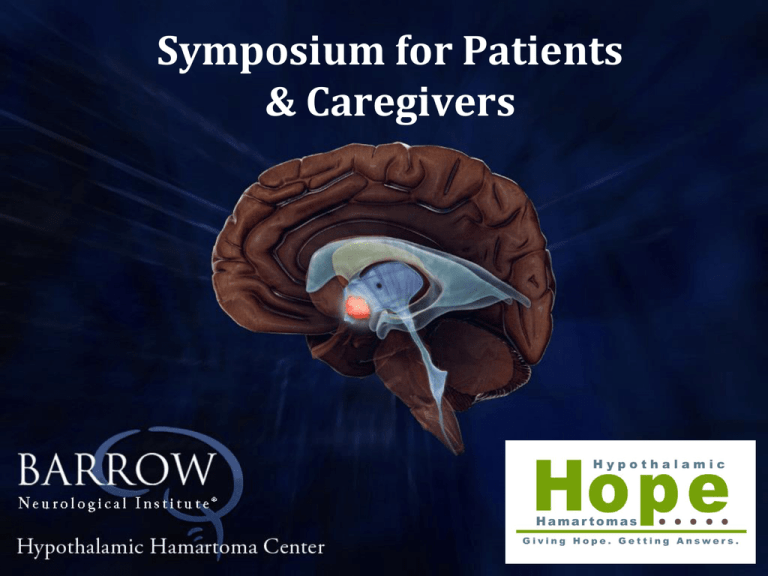
Symposium for Patients & Caregivers Hormonal Imbalances Laura Knecht, MD Adult Endocrinologist Medical Director, Barrow Pituitary Center Functions of the Hypothalamus • Secretes hormones-releasing and inhibitory effects on the pituitary gland • • • • • • • • Anti diuretic hormone (ADH) Dopamine Oxytocin Somatostatin Corticotropin Releasing Hormone (CRH) Thyrotropin Releasing Hormone (TRH) Gonadotropin Releasing Hormone (GnRH) Growth Hormone Releasing Hormone (GHRH) Anti Diuretic Hormone (ADH) • • • • ADH (vasopressin) made in the hypothalamus ADH stored in posterior pituitary gland Works at kidney to resorb water Reabsorbing water regulates sodium levels in the blood • Lack of ability to reabsorb water leads to increased thirst and urination Dopamine • Released by the Hypothalamus • Travels down the pituitary stalk • Continuous release inhibits the release of prolactin from pituitary Oxytocin • Acts at breast for milk let-down • Acts at uterus to aid in contractions Somatostatin • Inhibits growth hormone release from pituitary • Inhibits TSH release from pituitary Corticotropin Releasing Hormone (CRH) • Acts at pituitary to release adrenocorticotropic hormone (ACTH) • ACTH acts at adrenal glands to secrete cortisol (stress hormones) Thyrotropin Releasing Hormone (TRH) • Acts at thyroid to secrete TSH (Thyroid Stimulating Hormone) • Acts at pituitary to release prolactin • TSH acts at thyroid to release T4, T3 which controls metabolic activities Gonadotropin Releasing Hormone (GnRH) • Acts at pituitary to secrete FSH (Follicular Stimulating Hormone) and LH (Luteinizing Hormone) • Acts at ovaries and testicles to secrete Estrogen, Progesterone, and Testosterone Growth Hormone Releasing Hormone (GHRH) • Acts at pituitary to secrete Growth Hormone • Growth hormone acts at liver to produce IGF-1 • Acts at bones, muscles, cartilage Growth Hormone Deficiency • • • • • • • • In children, short stature Diminished muscle mass Increased fat mass Increased LDL Increased inflammatory markers (IL-6, CRP) Increased cardiac disease Decreased bone mineral density Diminished quality of life Treatment • Growth hormone deficiency • • • • • Recombinant human growth hormone Increased muscle mass Decreased fat ? Improvement in bone mineral density Improved quality of life Hypogonadism • Causes hypogonadism • In women • Inability to ovulate • Oligo/amenorrhea • Estradiol deficiency • Decreased bone mineral density • In men • Testicular hypofunction • Infertility • Decreased testosterone (energy/libido) • Decreased bone mineral density Treatment • LH/FSH deficiency • Men - testosterone replacement if not interested in fertility • Cannot follow LH • If interested in fertility, can be treated w/ gonadotropins or GnRH, HCG • Check sperm count • Women - estradiol-progestin replacement if not interested in fertility • If interested in fertility, can be treated w/ pulsatile GnRH or gonadotropins • Effects of testosterone still being studied Prolactin/Oxytocin Deficiency • Inability to lactate after delivery • Difficulty with uterine contractions Treatment • Not available • Not indicated Hypothyroidism • • • • • • • • • Central hypothyroidism Fatigue Heat/cold intolerance Decreased appetite Puffy face Dry skin Bradycardia Relaxation of deep tendon reflexes Anemia Treatment • TSH deficiency • Levothyroxine (synthroid, levoxyl, unithroid, armour) • Normalize free T4 – mid range (TSH not helpful) • Treat adrenal insufficiency first Adrenal Insufficiency • Cortisol deficiency • Mild • • • • • • Fatigue Anorexia Weight loss Decreased libido Hypoglycemia Eosinophilia • Severe • Vascular collapse • Loss of peripheral vascular tone • Death Treatment • ACTH deficiency • Administer hydrocortisone • 20-30 mg/d in varying regimens • Dexamethasone/prednisone (0.5-1mg, 5-7.5mg) have longer action • Increase in times of stress • Cannot measure serum ACTH, cortisol, urinary cortisol • Mineralocorticoid replacement unnecessary • Can unmask central DI w/ polyuria • Can increase blood pressure, renal flow, and decrease bone mineral density Diabetes Insipidus • Can occur prior to surgery, around time of surgery, after surgery • Can be temporary or permanent Diabetes Insipidus - Symptoms • Increased thirst • Craving ice water • Increased urination • Every 30-60 minutes • Night time urination 5-6x/night • Increased sodium levels • Above upper limit of normal Diabetes Insipidus - Treatment • If intact thirst center, can drink • Can drink to thirst • Usually desire ice water • Avoid significantly increased sodium loads • Tomato juice, V8, pickles, high salt foods Diabetes Insipidus - Treatment • If hypothalamus damaged, may not have desire to drink • Can schedule drinking times • With meals, at mid-morning (10am), mid-afternoon (3pm) Diabetes Insipidus – Treatment DDAVP (Desmopressin) • Oral • 0.1-0.2mg by mouth 2-3x/day • Half-life of 8-12 hours • Intranasal • • • • 10mcg spray 1-2 sprays 2-3x/day Longer half-life of 12 hours More potent Need to coordinate inhalation Diabetes Insipidus – Treatment DDAVP (Desmopressin) • Subcutaneous • Rarely necessary as outpatient • Avoids absorption issues • IV • Avoids absorption issues • Used in hospital around time of surgery A Special Thanks to our Sponsors • Aesculap • Barrow Neurological Institute @ St. Joseph’s Hospital • Barrow Neurological Institute @ Phoenix Children’s Hospital • Great Council for the Improved • Hope for Hypothalamic Hamartoma Foundation • KARL STORZ Endoskope