Pediatric History
Adapted from Davies’ Pediatric Chiropractic,
Ch. 2 & Mosby’s Guide to Physical Examination,
6th Ed., Ch. 1
Fundamentals of
Diagnosis
•
•
•
•
Skillful history-taking
Careful physical exam
Keen powers of observation
Wise selection of “other exams”
• x-ray, labs, etc.
• Good clinical judgment
LOOK – LISTEN – FEEL…
“More errors are made because of
inadequate history-taking and superficial
exam than any other cause.”
Tips…
Definite No-No’s
• Never be critical of another practitioner’s
diagnosis or treatment suggestions
• Never allow a child who has been brought
to you for care to leave without it
– do what you have to do, despite protests from
the child
• Never allow a child to be rewarded for
being sick
Discussing Difficult
Subjects
sexuality
abuse
serious disease
psychological etiology
suicide
divorce
drug addiction
peer issues
“I need to ask you some personal
questions, is that OK?”
“I know some things are difficult to
talk about and I really wish I didn’t
have to ask but I need to know
about…, is that OK?”
“Take all the time you need, I know
this is difficult for you.”
Be Aware…
“I want to talk to you about
something, but… I want to be sure
that you will not tell anyone.”
Recording the Pediatric
History
Reliability of the Historian
• “Historian” is any person providing
historical data
– describe by name and/or relationship to
the patient
– also record “reliability”
What is greater than God,
More evil than the devil?
The poor have it,
The rich need it,
And if you eat it, you die?
Answer: Nothing!
History
• The history for an infant or child will
be modified according to age
The following is just an outline…
Chief Complaint
• May be taken from a parent or
guardian
– Note the name, relationship & reliability
of the person providing the history
– The child should be included as much as
possible
– Appropriate for his/her age
Present Problem
• Note the “degree and character” of
the reaction to the problem
– Both parent and child
Different aspects of the history
assume or lose importance depending on
the age of the patient or the nature of
the problem.
Reserve detailed questioning for those
aspect s most pertinent to the child.
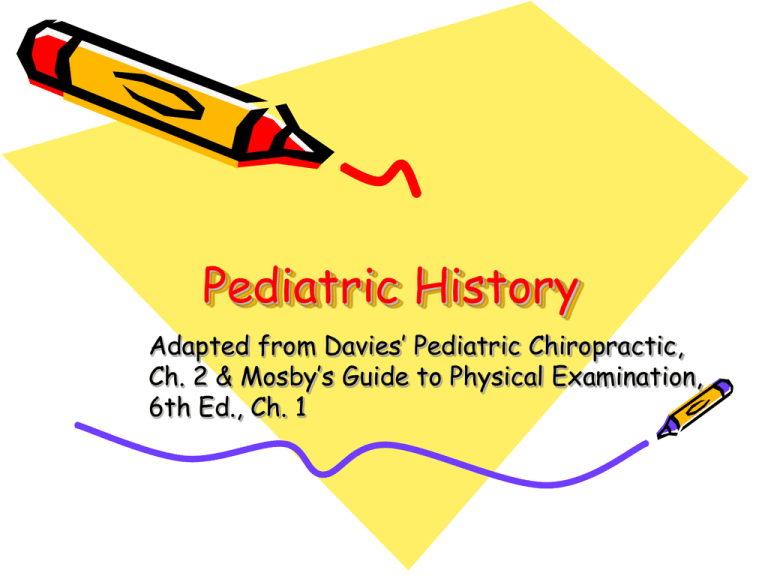
Past Medical History
• General Health and Strength
Past Medical History
• Mother’s Health During Pregnancy
– General health, extent of prenatal care
– Specific diseases or conditions
•
•
•
•
•
Infectious diseases (gestational month)
Weight gain
Edema, hypertension, proteinuria
Bleeding (approximate time)
Pre-eclampsia
Past Medical History
• Mother’s Health (cont’d)
– Medications hormones, vitamins, special
or unusual diet, general nutrition status
– Quality of fetal movement; time of onset
– Emotional and behavioral status
• Attitudes toward pregnancy and children
– Radiation exposure
– Use of alcohol or elicit drugs
Past Medical History
• Birth
– Duration of pregnancy
– Place of delivery
– Labor
•
•
•
•
spontaneous or induced
duration
analgesia or anesthesia
complications
Past Medical History
• Birth (cont’d)
– Delivery
•
•
•
•
presentation
forceps, vacuum extraction
vaginal or cesarean section
complications
– Condition of infant, onset of cry, APGAR
scores (if available)
– Birth weight of infant
Past Medical History
• Neonatal Period
– Congenital anomolies
– Baby’s condition in hospital, oxygen
requirements, color, vigor, cry, feeding
– Duration of baby’s stay in hospital;
infant discharged with mother?
– Bilirubin phototherapy
– Prescriptions (antibiotics)
Past Medical History
• Neonatal Period – First Month of Life
–
–
–
–
–
Jaundice, color
Vigor of crying
Bleeding
Convulsions
Other evidence of illness
Past Medical History
• Neonatal Period – Early bonding
– Opportunities at birth and during the
first days of life for the parents to
hold, talk to, and caress the infant
– Opportunities for BOTH parents to
relate to and develop a bond with the
baby
Past Medical History
• Feeding
– Breast or bottle (type of formula)
•
•
•
•
Reason for changes, if any
Frequency of feedings
Amounts offered and consumed
Weight gain
Past Medical History
• Feeding (cont’d)
– Present diet and appetite
•
•
•
•
•
•
•
•
Age of introduction of solids
Age child achieved 3 feedings per day
Present feeding patterns
Elaborate on any feeding problems
Age weaned from breast or bottle
Type of milk and daily intake
Food preference
Ability to feed self
Past Medical History
• Development
– Commonly used developmental milestones
NOTE:
• Parents my have baby books which can
stimulate recall
• Photographs may be helpful
Past Medical History
• Development (cont’d)
– Age when able to…
•
•
•
•
•
•
•
Hold head erect when in sitting position
Roll from front to back; back to front
Sit alone; unsupported
Stand with support; without
Use words
Talk in sentences
Dress self
Past Medical History
• Development (cont’d)
– Age when toilet trained
• Approaches to and attitudes toward toilet
training
– Dentition
• Age of first teeth
• Loss of deciduous teeth
• Eruption of first permanent teeth
Past Medical History
• Development (cont’d)
– Growth
• changes in rates of growth or weight gain
– Sexual
• Present status, any concerns
– Female: breast development, sexual hair, acne,
menstruation (description of menses)
– Male: sexual hair, voice changes, acne, nocturnal
emissions
– School
• Grade, performance, problems
Past Medical History
• Illnesses
–
–
–
–
Vaccinations
Communicable diseases
Injuries
Hospitalizations
Family History
• Maternal gestational history
– List all pregnancies
• Health status of living children
• Deceased children: date, age, and cause of death
• Miscarriage: dates and duration of pregnancies
• Age of parents at the birth of this child
*Review at least 2 generations on
each side of the family.
Personal and Social
History
• Personal status
– Nail biting, thumb sucking, breath holding,
temper tantrums, pica, tics, rituals, etc.
– Bed wetting, constipation, or fecal soiling of
pants
– School adjustment
“A day in the life of the patient” is often
helpful in providing insights.
Personal and Social
History
• Home Conditions
– Father’s and mother’s occupations
– Principal caretaker(s) of the child
• Daycare?
– Parents divorced or separated
– Food prepared by whom
– Sleep habits; sleeping arrangements
• In addition to the usual concerns,
inquire about any past medical or
psychological testing of the child
–
–
–
–
First visit to the dentist? optometrist?
Hearing checks?
Speech therapist?
Etc.
Review of Systems
• Skin
– Eczema; seborrhea (“cradle cap”)
• Ears
– Otitis media (frequency and laterality)
• Nose
– Snoring, mouth breathing
– Allergies
• Teeth
– Dental care
Adolescents
• Use open-ended questions
• Don’t force the adolescent to talk
Sometimes, allowing an opportunity
to write a concern may help.
Adolescents
Common Issues
H
E
A
D
S
Home
Education
Activities, affect, ambition, anger
Drugs
Sex
Adolescents
Common Issues
P
A
C
E
S
Parents, peers
Accidents, alcohol & drugs
Cigarettes
Emotional issues
School, sexuality