module h - Macomb
advertisement
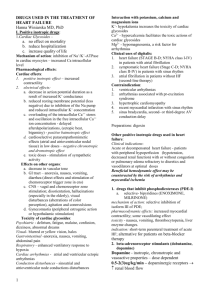
CARDIOVASCULAR AGENTS MODULE H Objectives • The student will be able to: • Define inotropic and chronotropic. • List those cathecholamines classified as Inotropic Agents. • State the formula for calculating blood pressure. • Describe how cardiac output is determined. • Describe how an increased or decreased systemic vascular resistance will affect blood pressure. • State the names and associated cardiac function of each of the waves seen on a normal ECG tracing. • List the two types of cardiac cells. • Define tachycardia and bradycardia. Objectives • State the primary drug used treat a bradycardia. • State the calcium channel blocker used to decrease tachycardia. • List the primary antiarrhythmic drugs covered in class. • List the most common medication used to treat ventricular ectopy. • List the primary antihypotensive agents discussed in class. • Describe how the effects of dopamine are dosage dependent. • State a vascular agent that is used in a hypertensive crisis. • State the beta-blocker used to treat hypertension. Objectives • Describe why bronchodilators may lose effectiveness when given to a patient on a beta-blocker therapy. • Define angina. • State the primary pharmacologic therapy used to treat angina. • Describe the pharmacologic action of nitrate therapy. • List the cardiac glycosides and describe when they are indicated in the clinical setting. • Name two anticoagulants and an antidote for each. • Name the three thrombolytics used to treat myocardial infarctions, strokes and pulmonary embolism. Definitions • Inotropic: Agents that affect the force of contraction. • Positive: Increased force of contraction. • Negative: Decreased force of contraction. • Chronotropic: Agents that affect the rate of contraction (heart rate). • Positive: Increases heart rate. • Negative: Decreases heart rate. • Tachycardia: Heart rate greater than 100/min. • Bradycardia: Heart rate less than 60/min. Adrenergic and Cholinergic Blood Pressure • Blood Pressure = Cardiac Output x Systemic Vascular Resistance • Since Cardiac Output is equal to SV x HR, BP = SV x HR x SVR • Medications that regulate blood pressure: • Increase/Decrease the stroke volume • Increase/Decrease the heart rate • Increase/Decrease the SVR Cardiac Glycosides • • • • Derived from Foxglove plant. Positive Inotropic Effect Negative Chronotropic Effect Used in the treatment of Congestive Heart Failure (CHF) • Cart vs. Horse • Examples • digitalis • digoxin (Lanoxin) • digitoxin Cardiac Stimulants • • • • Positive Inotropic Effect Positive Chronotropic Effect Adrenergic Agents Example • • • • epinephrine (First drug for all pulseless patients) dobutamine (Dobutrex) dopamine (Inotropin) isoproterenol (Isuprel) • Rarely used because of increased oxygen consumption. Positive Chronotropic Agents • Increase Heart Rate • Usually no effect on force of contraction. • Used to treat bradycardias and heart blocks. • Example • Atropine Sulfate Antihypertensive Agents • Used to reduce blood pressure. • Vasodilators • hydralazine (Apresoline) • nitroglycerine • nitroprusside (Nipride) • Beta Blockers • propanolol (Inderal) • verapamil (Calan, Isoptin) • Can be problematic with patients with reactive airways. ACE Inhibitors • Function by inhibiting the conversion of Angiotensin I into Angiotensin II. • ACE Inhibitors • captopril (Capoten) • benazepril (Lotensin) • enalpril (Vasotec) • Angiotensin II Receptor Blockers • valsartan (Diovan) • olmesartan medoxomil (Benicar) Antihypotensive Agents • Vasopressors • Used to raise blood pressure during shock states. • Examples: • Norepinephrine (Levophed) • Dopamine (Intropin) • Dopamine is dose dependent • Low Dose (1-2 mg/kg/min): Vasodilatation • Medium dose (2-10 mg/kg/min): Positive Inotropic Effect • High dose (>10 mg/kg/min): Vasoconstrictor Anti-anginal Agents • Increase coronary blood flow. • Coronary vasodilator. • Used during anginal attacks. • Angina: A heart condition marked by paroxysms of chest pain due to reduced oxygen to the heart. • Nitrates (nitroglycerin) • Can cause an increase in methemoglobin. • Beta Blockers • propanolol (Inderal) • Calcium-Channel Blockers • verapamil (Isoptin, Calan) Conduction System of the Heart Ectopic Foci • When an impulse originates from outside the normal conduction pathway it is said to be ectopic. • These impulses arise at any time during the conduction cycle. • They are responsible for irregular heart beats. • They can arise from tissues in either the atrial or ventricular wall. Electrocardiogram (ECG) • ECG Tracing • • • • • P wave P-R interval QRS complex ST segment T wave Antidysrhythmic Agents • Drugs that suppress cardiac dysrhythmias. • Example of dysrhythmia is a Premature Ventricular Contraction (PVC). • Examples: • • • • • Lidocaine (Xylocaine) Pronestyl (Procainamide) Amiodarone (Cordarone) Adenosine (Adenocard) Verapamil (Calan) • Side effects of these agents include hypotension and conduction defects (heart blocks). Anticoagulants • Used to manage blood clots. • Examples • Heparin • Warfarin (Coumadin) • High risk of bleeding. • Use with caution after prior-surgery. • Increased risk of hemorrhagic stroke. • Antidote: • Heparin: Protamine Sulfate • Warfarin: Vitamin K Thrombolytic Enzymes • Used to break up existing clots. • Multiple generations with each being “better” than the previous. • Examples • • • • Alteplase (Activase) tPA Reteplase (Retavase) tPA Urokinase Streptokinase