PGDs and Champix
advertisement
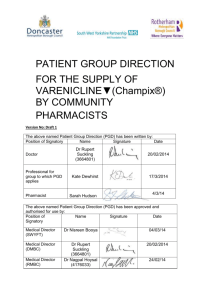
An introduction to PGDs and Varenicline Sarah Hudson, Acting Chief Pharmacist Objectives for this afternoon • PGDs in practice • Varenicline What is a PGD? • A written instruction for the supply or administration of a medicine to a group of patients who may not be individually identified before presentation for treatment. • Replace standing orders, group protocols, unit/department procedures, etc. • These are now unlawful. • Supply of a POM or P other than on prescription or PGD is a criminal offence. Background • Before PGDs, law was unclear. • Practitioners administering POMs not on individual prescription were probably breaking the law (Medicines Act 1968). • Crown 1 recommended clarification. • Law changes came into effect August 2000. What do PGDs permit? • Authorise named professionals from specified groups to supply or administer POMs other than on individual prescription from a doctor in specific circumstances. • Supply/administration, not prescribing. • Empowering for non-prescribers. • Opportunity to ensure best practice. What does this mean in practice? PGDs specify • What registered professional group can use the PGD e.g. Pharmacists. • In what situations. • Inclusion and exclusion criteria (how would you check). • Product to be used. • Follow up. When to use a PGD • Most patients should be treated on an individual, patient-specific basis. • “Use PGDs in limited situations where there is an advantage for patient care”. • Patient safety must not be compromised. • Must be consistent with appropriate professional relationships & accountability. How to use a PGD • Pharmacists must work in line with GPhc Professional Standards. • PGD must be authorised for your organisation. • You must sign the PGD. How to use a PGD • No scope for interpretation, discretion or adjustment. – This is not prescribing, it is supply/administration. • A patient excluded from treatment under a PGD might still be treated, but only on prescription from a doctor or non-medical prescriber if applicable. How are PGDs produced? • Specific requirements in legislation. • Must be produced by a doctor, pharmacist and member of profession to which applies. • Must be authorised for use by specified senior staff. Labelling of medicines • Must use original packs (eg Levonelle) or use pre-packs from a pharmacist unless giving for immediate administration or be labelled as per labelling legislation. • All patients should be given the manufacturer’s patient information leaflet. Other responsibilities • Signing up mechanism required. • Named person to be responsible for maintaining the file. • System for review and updating. • Distribution. • Questions? Completing the voucher • The Stop Smoking Advisor (Specialist Service or LES) will complete the first 3 sections of the voucher – client details, advisor details & request titration or maintenance pack • The dispensing pharmacist must complete the date of supply, inclusion/exclusion criteria, client consent and sign the voucher at the bottom of the form. Inclusion/exclusion criteria 1. Aged 18 or above 2. Tobacco dependant & sufficiently motivated to stop smoking 3. Agreed to behavioural support during course of Varenicline Is the client currently: 4. Pregnant or breastfeeding? Does the client have a history of: 5. Renal disease? 6. Epilepsy? 7. Sensitivity to Varenicline or any of its excipients? 8. Psychiatric illness? All clients must answer YES to Questions 1-3 to be eligible. If clients answer YES to any of Questions 4 -8, not eligible for Varenicline via the PGD. Quick Questions?? 1) According to the PGD what would you supply on the 1st Supply? 2) What would you do if the person arrives for the second supply 4 weeks after receiving supply 1? 3) Can you issue varenicline under a PGD you haven’t signed? 4) Can you supply to a pregnant woman under this PGD? 5) Can you supply if the person indicates they wont access behavioral support? Useful resources www.medicines.org.uk www.bnf.org Varenicline (Champix) ▼ • CHAMPIX is indicated for smoking cessation in adults. • Black triangle status and MHRA advice. • http://www.mhra.gov.uk/Safetyinformation/DrugS afetyUpdate/CON087901 Dose • The recommended dose is 1 mg varenicline twice daily following a 1-week titration as follows: Days 1 – 3: 0.5 mg once daily Days 4 – 7: 0.5 mg twice daily Day 8 – End of treatment 1 mg twice daily Treatment • The patient should set a date to stop smoking. CHAMPIX dosing should usually start at 1-2 weeks before this date. • Patients who cannot tolerate adverse reactions of CHAMPIX may have the dose lowered temporarily or permanently to 0.5 mg twice daily. • Patients should be treated with CHAMPIX for 12 weeks. Effect of smoking cessation Physiological changes resulting from smoking cessation, with or without treatment with CHAMPIX, may alter the pharmacokinetics or pharmacodynamics of some medicinal products, for which dosage adjustment may be necessary (examples include theophylline, warfarin and insulin). Neuropsychiatric symptoms • Changes in behaviour or thinking, anxiety, psychosis, mood swings, aggressive behaviour, depression, suicidal ideation and behaviour and suicide attempts have been reported in patients attempting to quit smoking with CHAMPIX. • Depressed mood, rarely including suicidal ideation and suicide attempt, may be a symptom of nicotine withdrawal. Cardiovascular events • Certain cardiovascular events were reported more frequently in patients treated with CHAMPIX. • Patients taking CHAMPIX should be instructed to notify their doctor of new or worsening cardiovascular symptoms and to seek immediate medical attention if they experience signs and symptoms of myocardial infarction or stroke. Reporting adverse reactions • Compliance and adverse reactions will be monitored at the bi-weekly follow-up. • Staff will report all adverse reactions in accordance with the UK Adverse Drug Reaction Reporting Guidelines (Yellow card system available at; http://www.yellowcard.gov.uk/). • Clients who report agitation/ depression/ suicide ideation /change of mood or new or worsening cardiovascular symptoms must stop treatment immediately and seek prompt medical advice. Any Questions or Comments?