Complaints in the NHS - Awes Siddique
advertisement
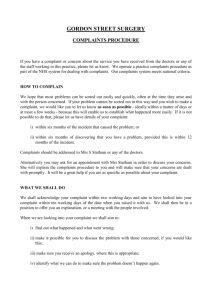
Complaints in the NHS Awes Siddique STGP1 “ Patients who complain about the care or treatment they have received have a right to expect a prompt, open, constructive and honest response including an explanation and, if appropriate, an apology. You must not allow a patient’s complaint to affect adversely the care or treatment you provide or arrange.” GMC (Good Medical Practice) Objectives Burden and impact of complaints Measures to avoid complaints and potential claims Legislation 133,600 NHS complaints in 2007 – 32% linked to Primary Care New regulations governing NHS complaints in England came into force on 1 April 2009 following the White Paper commitment to develop a single comprehensive complaints procedure across health and social care by 2009 The Local Authority Social Services and National Health Service Complaints (England) Regulations 2009 Aim to make complaints handling open and accountable, fair and proportionate, and patient-focused – with a view to seeking continuous improvement. Oblige NHS organisations to have arrangements in place to deal with patient complaints Sets out the following rights for patients: You have the right to have any complaint you make about NHS services dealt with efficiently and to have it properly investigated. You have the right to know the outcome of any investigation into your complaint. You have the right to take your complaint to the independent Health Service Ombudsman, if you are not satisfied with the way your complaint has been dealt with by the NHS. Competence Always act within your limitations Never undertake a task that is beyond your competence Chaperone Applies whether or not you are the same gender Always document when a chaperone is offered and declined Confidentiality 1998 Data Protection Act GMC guidance (Confidentiality: Protecting and providing information) Take steps to avoid potential leaks Reception areas – overhearing sensitive info Restricted access to electronic records to only those who require it Encryption software Consent GMC guidance Capacity Always obtaining consent – even for the briefest of physical examinations! Civil claim in negligence/ assault Clinical Records “You must keep clear, accurate and legible records, reporting the relevant clinical findings, the decision made, information given to the patient, and any drugs prescribed or other investigation or treatment” GMC Never rewrite notes at later date – make clear any retrospective entries by signing and dating alterations Patients have legal right to access their records Avoid derogatory statements, offensive patient acronyms and criticism of colleagues! Careful prescribing 25% of NHS claims from prescribing errors Generic drug names In accordance with BNF Commonest errors Wrong dosage Inappropriate medication Failure to monitor treatment (SEs and toxicity) Communication failure Conduct 20% of all complaints about GPs in 2007 were in response to poor attitude Calm, sympathetic and professional manner ‘Physician-Patient Communication’ – Drs who never received a claim used humour and laughed more and spent approx 3 min longer per consultation Cover Check with your medical protection organisation for appropriate cover to reflect the work you do Communication 43% of complaints to Healthcare Commision were related to limited discussion about treatment options Cover your back Seek advice from senior colleagues or your medical protection organisation Respond promptly Finally In 2002, 72 per cent of people were very or quite satisfied with their local NHS doctors or GPs In 1 in 10 cases referred to the Healthcare Commision (2007-8) – the complainent was simply seeking apology or an acknowledgment that the care could have been improved Survey of MPS members revealed that 90% believed an explanation and apology reduced potential for complaints Saying sorry doesn’t necessarily equate to admitting liability Thank You! …..any complaints?