Click here to view the presentation slides
advertisement

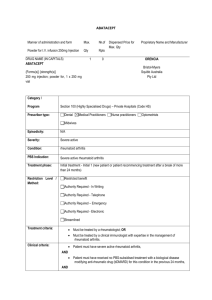
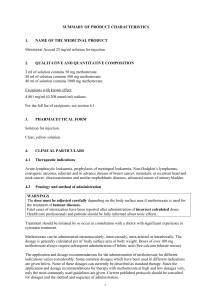
Drug treatments for Rheumatoid Dr Steve Jones Consultant Rheumatologist 15 March 2012 Drug action (1) – Enzyme blockers Enzymes – chemical reactions cell metabolism Examples: Methotrexate Non-steroidals Drug action (2) – cell signalling (e.g. hormones, growth factors, immune system) Examples: Positive signal Steroids Codeine Signal blockers Anti-TNFs Drug effect depends on concentration … … determined by balance intake & metabolism Science Recap Most drugs work by blocking enzymes (cell function/metabolism) or interfering with cell signalling (increase/decrease) Drugs work best at specific concentration in body/tissues - Need for regular dosing - Differences in absorption/breakdown (genetics, disease) affect ‘steady state’ concentration too low ineffective: too high side effects Some drugs are “stored” in body tissues prolonged effect (Methotrexate - 1-2 weeks. Bisphosphonates (Alendronate etc) weeks, months) Analgesics “pain killers” - work on brain, not joints. Paracetamol - max 4g daily (overdose liver damage) • safe but weak analgesic Opiates - derivatives of Morphine (‘opium’) • naturally occurring system “endorphins” (pain/stress response) • act via receptors on nerve cells - pain system + others • including nerve cells controlling gut propulsion. Opium poppies Opiates – potency weak medium Dextropropoxyphene Dihydrocodeine Codeine Tramadol Buprenorphine strong Fentanyl Morphine Oxycodone Depends on dose: 200mg Codeine = Max 1.2x 100mg Tramadol = 10mg MST (Morphine) Max 4x Max 20x (+) Traditional : ‘Pain ladder’ – escalate between groups But : M, K, D receptor types Codeine, Tramadol – M, Buprenorphine – Dm, Oxycodone – Km overlap use in combinations Opiates (3) Fixed combinations with Paracetamol • ALL MAX 8/d Co-codamol (Codeine/Paracetamol) 8/500 (8mg Codeine, 500mg Paracetamol) - non-prescription 15/500 (15mg Codeine) 30/500 branded- Kapake, Solpadol, Tylex : identical Co-dydramol (Dihydrocodeine/Paracetamol) 7.6/500 - non-prescription 10/500 (usual) - equivalent to Cocodamol 15/500 20/500 “Remedeine” (equivalent to Kapake) Tramacet (37.5mg Tramadol/325mg Paracetamol) Opiate Combinations: Plusses - easy to take Minuses - possible Paracetamol overdose >8/d Inadequate analgesia (8,15,30?) Inflexible dosing In higher strengths (e.g. Cocodamol 30/500) : one tablet every 2-3 hours better than 2 every 4-6 Opiates (5) S/E: • nausea, constipation – GI • drowsiness – brain • skin (nerves) – itching (antihistamines) Constipation - worst with Codeine use softeners (eg lactulose) , and laxatives (senna) ‘Targinact’(Oxycodone + Naloxone) – expensive! ?addiction - rare - psychological “abuse” high doses/long time - physical: “cold turkey” dependence ≠ addiction Alternate delivery systems: Patches - drug enters bloodstream through skin Buprenorphine (BuTrans, Transtec) Fentanyl (Durogesic) • less GI S/E • convenient (1, 2/week : variable doses) • occasional skin reactions, can fall off • relatively expensive Sublingual – under tongue (Buprenorphine) Buccal – inside cheek (Fentanyl – cancer pain only) rapid blood peak (often causes nausea) Suppositories (Morphine) NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) - symptomatic treatment Related chemically to Aspirin Weak analgesic (= Paracetamol, low dose Codeine) – brain, joints Antipyretic (fever) - brain Anti inflammatory – joints • Use instead of / additional to Paracetamol, Opiates NSAIDs work by : Inhibiting COX enzyme (produces “prostaglandins”) - increase bloodflow and tissue fluid (inflammation) => swelling, heat & stiffness - sensitise pain nerves (inflammation) BUT: COX also – • needed for gastric mucus production “COX1” (dyspepsia, ulcers, stomach/bowel bleeding) • needed for kidney blood flow regulation (hypertension, fluid retention, kidney impairment) • involved in blood clotting (platelets) (heart attack & strokes) NSAIDs (3) “Standard”: Ibuprofen, Diclofenac, Naproxen, Indometacin “COX2”: ‘coxibs’ Meloxicam (?) Rofecoxib (Vioxx) - withdrawn (& others) Etoricoxib - (Arcoxia) Celecoxib (Celebrex) Coxibs “kinder on stomach” but: standard NSAID + Omeprazole cheaper routine - age > 60, history indigestion/ulcers NSAIDs (4) Benefits - additional pain relief, good for swelling/stiffness Problems - Control symptoms of inflammation only, not process (exception- gout) Anti-inflammatory potency = Side effect potency Cardiovascular S/E – Small increase heart attacks, strokes (controversial!) ?Naproxen, lower doses safest Interfere with Aspirin for angina Aggravated by hypertension & fluid retention Corticosteroids (“steroids”) Prednisolone : Deflazocort : Dexamethasone Mimic Cortisol (naturally occuring steroid hormone) • produced from adrenal glands Basal - essential to health (= 1-2.5mg Prednisolone/d) (normal cell metabolism, blood pressure, salt balance) Elevated stress response (infection, trauma..) Mobilises sugar + fat + protein reserves (repair) Anti-inflammatory. Anti-fatigue. Increases appetite. Steroid Effects: Low doses (7.5mg or less) - Anti-inflammatory (cell function and mobilisation) Higher doses - Immunosuppressant Anti-allergy Uses: rheumatic diseases (RA, PMR, SLE…) inflammatory lung, liver, bowel, brain, muscle, skin disease Benefits : control disease process, not just symptoms = ‘DMARD’ rapid onset action (24-48 hrs) Steroids: Rheumatology Uses - courses for flares or disease stabilisation with DMARD Flares - usually only need 10-15mg Prednisolone daily (not 30mg given for COPD/asthma) Injections - IM - (Kenalog, Depomedrone) - typically last 4 weeks IA - into joints (4-6 wks : need control disease as well) Infusion (drip) - for severe flares as part of immunusuppressive regime (vasculitis, kidney disease) to reduce allergic side effects (Rituximab) Steroid S/E (1): “Cushings disease” - Excess Cortisol due to adrenal tumour permanent “stress response” • • • • • • Weight gain (appetite and metabolism changes) Thinning skin and bones/osteoporosis - muscle weakness - protein Increased blood sugar (diabetes) and fats (cholesterol) Insomnia and mood changes Dyspepsia and peptic ulcers (NSAID-like) High blood pressure, fluid retention • Increased infections (higher doses) skin, chest, urine (immunosuppression) Side effect risk = Dose x Time (patient sensitivity varies) Steroid Side Effects (2): “Addisons disease” - acute Cortisol deficiency (adrenal, pituitary gland damage LONG TERM STEROID USE) • inability to mount stress response to trauma, infections • severe lethargy, fatigue, hypothermia • low blood pressure, low blood sugar/salt • severe cases cardiovascular collapse DO NOT STOP STEROIDS SUDDENLY (“physical dependence”) - Carry Steroid card/alert bracelet - Only adjust steroid doses after medical advice - May need slow tail to stop (1mg/month reduction) - IV replacement (surgery) All patients on regular steroids need: monitoring blood pressure, sugar and cholesterol screening and treatment for osteoporosis prevention ? Omeprazole (PPI) for peptic ulcer prevention & regular review to minimise steroid dose/stop if possible Side effects unlikely from IA use (joint injections) - may get with repeated IM use DMARDs “Disease modifiers” Control underlying disease process. NOT CURE. Preventative - need taking regularly (even if disease inactive) Effects - slow acting (disease inflammation symptoms) - reduce symptoms and signs inflammation - reduce/prevent longterm joint damage (disability) - reduce medical complications (including heart) - reduce systemic upset (fever, anaemia, fatigue..) DMARD Types: 1) Chemicals (‘small molecules’) : taken orally Methotrexate, Azathioprine, Leflunomide, Cyclophosphamide “antimetabolites” Block enzymes involved in cell growth/division main effects on actively dividing cells • • • • • Immune cells (lymphocytes) - desired effect Bone marrow (white blood cells, red cells) Gut lining cells. Liver cells (metabolically active) Cancer cells (chemo) Foetus Hence side effects - GI upset (dyspepsia, nausea, mouth ulcers, diarrhoea) Blood problems (anaemia, low WCC, platelets) Liver inflammation (Methotrexate & alcohol also) (Leflunomide & ?Infections Avoid pregnancy (Azathioprine relatively safe) Side effects worse with higher doses need slow dose escalation Also problem with slow metabolisers: Azathioprine - genetic test Allopurinol Methotrexate - kidney disease NSAID. Age Leflunomide - excreted in bile and reabsorbed (drug persists even when stop taking) Use - singly, work better in combination Methotrexate and Leflunomide most effective Methotrexate best tolerated antimetabolite (+ Folic Acid) Other DMARDs (weaker - different mechanisms) - Mild disease or drug combinations • Sulfasalazine - salicylate and antibiotic (rash) • Gold & Penicillamine - kidney problems, rashes • Hydroxychloroquine – eye (rare) Advantages – Oral Relatively effective Cheap Variable dosing Infection rate similar (stop in severe) Disadvanges Slow onset action (weeks) GI side effecs common (?switch to injectable) Variation Methotrexate absorption ‘Antimetabolite’ effect limited by S/E ● Incomplete control of severe cases ● Incomplete prevention of joint damage Blood toxicity difficult to predict; rare cases fatal DMARD types 2) Proteins : “Biologics” Like insulin - produced by ‘genetic engineering’ “brewed” - cell culture, not chemically synthesised intrinsically expensive to produce All protein drugs digested by oral route (= “steak”) need giving parenterally (drip, subcut) BIOLOGIC DRUG TARGETS Types – Anti-TNFs (cell signal) Infliximab Etanercept Adalimumab Certolizumab Golimumab Anti B cell (antibodies) Anti T cell (“helper”) Anti IL6 (signal) Rituximab Abatacept Tocilizumab * ALL SUPPRESS IMMUNE SYSTEM FUNCTIONS * (Infection risk!) Biologics- Advantages: more effective than conventional DMARDs (symptoms, joint protection) Disadvantages: cannot be used together (with other biologics) increased common & rare infections (TB) Must stop drug during infection/surgery (flare risk) ? Patients with chronic infections (bronchiectasis, COPD, bone & joint, TB, hepatitis) COST - rationing (“NICE guidelines”) ?? long term side effects BSRBR Recap1: Analgesics (Pain killers) “as required” Paracetamol, Opiates Work on brain, not joints Work best taken regularly (as all drugs) when needed Can use opiates in combination (eg. Butrans patch and Cocodamol) NSAIDs (anti inflammatories ) “as required” Reduce pain, stiffness, swelling joints No effect on disease process/joint damage Improve quality of life/disability Common side effects due to natural function of drug (GI/ulcers; hypertension - fluid; bleeding/clotting problems) Cannot mix with each other (avoid Nurofen/Ibuprofen and Naproxen) Recap2: DMARDs (including steroids) - “regular” Control disease process, secondary benefits swelling and pain Slow acting. Can use in combination Variably reduce joint damage, medical complications Regular monitoring essential Gradual dose increase reduces S/E Slow tail off steroids (don’t run out!) Biologics: newer DMARDs Genetically engineered proteins (not oral) More effective, less side effects Use limited by expense Need to stop during significant infections May get “unusual” side effects (TB, MS) - but rare Recap3: OTHERS Coanalgesics (Amitriptyline, other antidepressants, Gabapentin etc) • Reduce “nerve pain” • Aid sleep (non-addictive) Drugs for medical complications - (control cholesterol & blood pressure; prevent osteoporosis) Supplements: Vit D/calcium Fish oils? Glucosamine/Chondroitin? Iron deficiency common (NSAIDs) SOME PRACTICAL ISSUES Avoiding Side Effects : Minor Is it due to drug? Common SE - Pharmacist/GP, ArthResUK leaflets, helpline Package inserts - list all possible side effects Statistical significance ≠ clinical (e.g. trial drug headache 15%, placebo 10% - only 1/3 HA due to drug) Is it due to formulation/brand? “Excipients” Could I get used to the drug? Reduce dose If in doubt: stop drug few days then rechallenge GI intolerance: Take with food (absorption) Injections Slower dose increase Patches Split dose (Methotrexate, Sulfasalazine) Enteric coated/slow release Alcohol and tobacco ……. GI intolerance with multiple drugs: Marker of underlying problem Hiatus hernia, reflux, ulcers, Helicobacter, IBS ?diet Can I reduce dose? Analgesics/NSAID - need may vary with time (flares/remissions/weather) Work quickly - no harm in temporary reduction Consider non-drug methods: (rest, relaxation, hot/cold, rubs, splints, TENS ……) DMARDs - ? lower dose combinations may reduce during remission, without flare Avoiding major S/E Illness, drug interactions & new medications (affect metabolism/drug levels) Fever/chest infections - dehydration Urine infections - transient reduction kidney function Antibiotics - liver test problems, direct drug interactions ‘Red flags’ • significant abdominal pain/jaundice • abnormal bruising or bleeding • serious or prolonged infection, high fever • unexplained breathlessness • protracted vomiting or diarrhoea • severe rash or oral ulceration Avoiding major s/e 2 Immunosuppressants/biologics: Immunisation status? (avoid live vaccines) Annual flu jabs Avoid contact with chickenpox/shingles Tropical disease risk (TB, Malaria…) Biologics - stop during any infection/prior to operations (especially orthopaedic) ** Attend regularly for blood monitoring checks ** Why is my drug not working? What are your expectations? DMARDs take weeks to work ……. Steroids are poor painkillers ….. Analgesics work better if taken regularly …… Is it really not working? Is the problem inflammation (stiffness, swelling) or pain (tenderness)? Is the problem due to my Rheumatoid? Coexisting or secondary osteoarthritis Back pain – usually isn’t Soft tissue problems (tennis elbow, bursitis) Why is my drug not working? 2 Are you taking enough (dose, route, genes, weight)? Primary vs secondary failure? DMARDs - rule of 1/3’s Biologics “diminishing returns” 1st-3rd anti TNF HACA - Infliximab NEW DEVELOPMENTS 1) Drug use Minimise Inflammation x Time reduces damage Early recognition RA and specialist treatment Objective measure disease activity (DAS) Frequent regular follow-up (early or persistent disease) “Treat to target” - remission ideally Use rapidly escalating dose of DMARD combinations - usually including Methotrexate Temporary use steroids for rapid control (IM > oral) Use minimum effective doses NSAID/anagesics - reduce s/e. 2) New Drugs Chemicals ‘small molecule’ : tablets - inhibitors of TNF production/metabolism (one effect of steroids…) several under investigation (lab/animal study) - lymphocyte activation blockers ‘JAK kinase inhibitor’ (Tofacitinib) available EU/UK late 2012 (then NICE..) ‘Syk kinase inhibitor’ (Fostamatinib) works in RA but unacceptable S/E 2) New Drugs Biologics - other cell signal blockers (immunosuppressants) IL6 (Tocilizumab) – in use IL23 (Ustekinumab) – psoriasis ? Psoriatic arthritis (trials) IL17 (Secukinumab) – trials RA, PsA, AS IL18 – under development * Potential problem – all similar to currently available drugs - ‘Biosimilars’ (? cheaper, treat more people) Enbrel patent to 2028 : Humira to 2017 - Denosumab (biologic osteoporosis treatment) high doses reduce RA bone erosion/joint damage (preliminary, not yet licenced for RA…) 2) New Drugs Cancer Biology (potential use in arthritis – yrs) Abnormal cell growth New blood vessels Connective tissue damage (tumour invasion & spread) e.g. experimental MMP’ase inhibitors (enzymes break down bone tumour spread, also RA erosions) - Lung cancer trials “Personalised medicine”? Gene screening for - best drug to use (speed of effect, cost) - reduced risk of side effects So far lots of research but no definite pointers (Rituximab - works better if seropositive- not absolute) Clinical research? best use of existing drugs (current order of biologics use in UK determined mainly by cost …)