Sedation and Analgesia in the ICU
advertisement
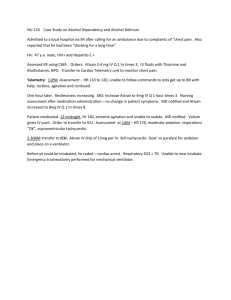
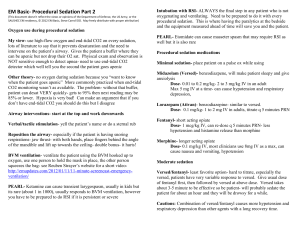
Sedation and Analgesia in the ICU 34 year old man was admitted to the intensive are unit 3 days ago for increasing respiratory failure from community acquired pneumonia. He is intubated and ventilated in an ARDSNet lung protective strategy and on 5 mcg/min of levophed. The bedside nurse calls you at 0342 because the patient is distressed. When you examine the patient, his eyes are open and he is pulling at the restraints. His blood pressure is 193/90, heart rate 120, respiratory rate 34, oxygen saturations 91%. Last ABG: pH 7.37, PCO2 43, PO2 84, BE-1. Physical exam is unchanged from your last examination in the morning. What are some physiological reasons for the patient’s current condition? You rule out any obvious physical causes for this behavior. What are 5 possible causes for patient distress? Anxiety Pain Delirium Dyspnea Neuromuscular paralysis while aware What is the definition of anxiety? What is the definition of delirium? State of apprehension and autonomic arousal in response to real of perceived threats. Acute, reversible, impairment of consciousness and cognitive function that fluctuates in severity. Can a patient with normal blood gases be dyspneic? Why? The patient is obviously not paralyzed and the nurse really wants you to do something as the patient is getting worse and becoming a danger to himself. What non-pharmacological methods of treating distress may help? Fix reversible causes identified Minimize irritating stimuli such as pulling on the ETT Reassurance Communication to and from the patient Family visits Sleep cycle hygiene Your attempts at reassurance has been met with marginal success. What four drug types are used to treat patient distress? Benzodiazepines Opiods Neuroleptics Propofol What is the mechanism of action of benzodiazepines? Are they indicated for anxiety, pain, delirium, dyspnea, or awake paralysis? What benzodiazepines are usually available in the ICU? How are they different from each other? What are the doses for each of these? What factors determine Ativan and Verseds’ differences between each other? Receptor binding affinity Lipophilicity Versed is more lipophilic and therefore crosses the blood-brain barrier faster giving it a more rapid onset. Can store in adipose tissue Elimination kinetics Ativan is higher and therefore is more potent. Versed undergoes rapid hepatic oxidation. Ativan has a low hepatic clearance and Vd and is glucuronide conjugation and excreted in the kidneys Why is Ativan not generally given by continuous infusion? What happens to the kinetics of Versed if given continuously over several days? Why? While you are up, another nurse approaches you about his patient. He is taking care of a 56 year old woman who is one day post op for a bowel resection due to ischemic colitis. The patient has awoken and complaints of diffuse abdominal pain particularly around the wound. She is hemodynamically stable and physical exam finds diffuse tenderness but no rebound or guarding. WBC is going down and her creatinine and ABG are normal. What are some causes for this pain? How do opiods work? What types of opiods are commonly used in the ICU? What is the usual dose range for bolus and infusion of morphine, fentanyl, and hydromorphone? What is the time to peak effect and elimination of each of these drugs? Why is transdermal fentanyl usually not used in the ICU? The nurse for the first patient comes over to get you. Her patient is now much more combative and confused after being given 2 mg of ativan twice in the last hour. Why is this patient more agitated? What alternative treatment can be used in this case? What is the mechanism of action of haloperidol? What is the usual dosage range for haloperidol? What is the half-life and elimination for haloperidol? What are the two most important side effects of haloperidol? Prolonged QT and Torsade de pointes Extrapyramidal effects As you are wandering back to bed, you check in on a patient who was admitted two days ago with epiglottis. She is sedated on a propofol infusion. What is the mechanism of action of propofol? What are the indications for propofol use in the ICU? What is the usual dose range for propofol? What are the contraindications for propofol? What are three of the most important side effects of propofol? Hypotension Hypertriglyceridemia Lactic acidosis and rhabdomyolysis Why is the patient’s urine bag green? How many calories/mL are in propofol? In the morning, you come back to see and examine your patient with agitation and pneumonia. He is now completely unresponsive to voice or pain. Overnight he has received 15 mg of ativan and 25 mg of haloperidol. His nurse now states that the patient is comfortable and wants to continue the current plan. What methods or tools can we use to measure depth of sedation? Consider SAS RASS MSAT MAAS How is the sedation tools at this site performed? What is a BIS monitor? What role do they have in the ICU? What are the consequences to oversedation in critically ill patients? What are some methods to avoid oversedation? Consider Intermittent bolus dosing, no continuous infusions Daily interruption of sedation What are the long term psychological consequences of ICU? PTSD Cognitive dysfunction Dementia Questions??