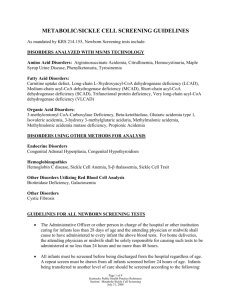
The Social Consequences of Expanding Newborn Screening
advertisement
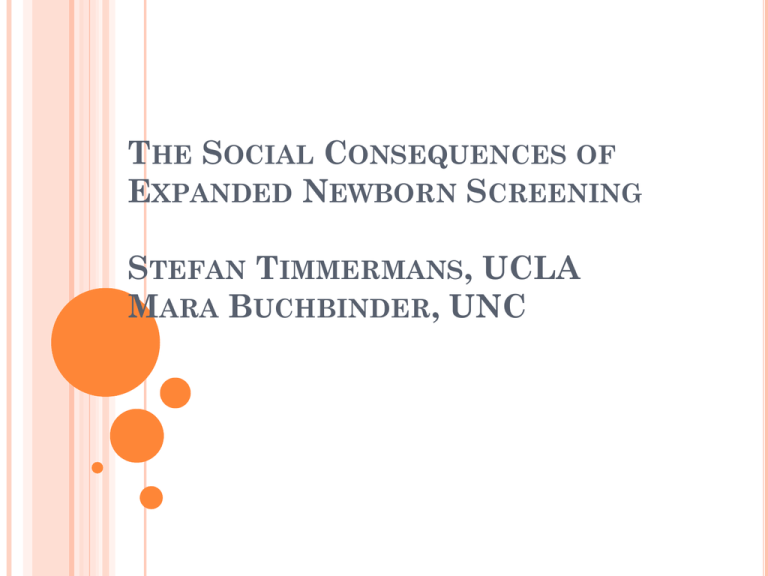
THE SOCIAL CONSEQUENCES OF EXPANDED NEWBORN SCREENING STEFAN TIMMERMANS, UCLA MARA BUCHBINDER, UNC 2009: 51 million people without health insurance Medicare for people over 65 Virtually mandatory universal newborn screening 99% of 4.1 million babies born annually Screened for 54-55 conditions Amazing political achievement Highest public health priority Highest health service priority NEWBORN SCREENING PKU screening in 1960 Ideal condition: prevent mental retardation Still, many unanticipated problems Cautious expansion State responsibility Pediatrics 2000;106:389-422 Copyright ©2000 American Academy of Pediatrics TANDEM MASS SPECTROMETRY EXPANDED NEWBORN SCREENING 2005 American College of Medical Genetics Recommend screening for 54 conditions 3 innovations Embrace MS/MS Create evidence Expand beneficiaries Baby Family Society Diagnostic odyssey Science Avoid preventable deaths SOCIOLOGICAL PROJECT: Do anticipated benefits for infant, family, and society correspond to reality? New patient population Saving lives? METHODOLOGY Qualitative research project Follow 75 families over 3-year period in metabolic clinic Audiotape-observe visits with genetics team Attend staff meetings-interview staff In-depth interviews with families in home Follow-up interviews Review medical records Diverse population Socio-economically Ethnicity Well-regarded genetics clinic 4 POSSIBLE OUTCOMES OF NBS Negative results (not in study) False positives: rarely in study True positive: either symptomatic or well-known Ambiguous out-of-range: patients-in-waiting Does the newborn have a disease? What is the disease the child has? PATIENT-IN-WAITING Suspended between disease and normalness Either biochemical artifact: false positive Or potentially life-threatening disease: true positive And no one knows what it is Contradictory messages Parents and newborn share patient role Shock no informed consent Retest ASAP Preventive measures He was five days old and we got a phone call from our pediatrician. We just talked to her about him sleeping through the night if that was even possible and she was like yeah go head try to do it. So she frantically called me when he was five days old and said don’t let him sleep through the night you have to feed him every three hours or basically he can die. That was pretty surprising and shocking. We had to take him when he was five days old to get his blood drawn and they did a blood test to reconfirm that he had a metabolic disorder. PATIENT-IN-WAITING: ONSET Pediatrician unfamiliar with condition Internet and health communications: worst case And actually the first time that they had suggested that he might have PKU, you go back to read the material and it’s like a blur. ...Basically, it says, we test for this. PKU is this, and basically in nutshell, because of a deficiency in an enzyme, your child can become mentally retarded. So, I’m like, what? And then you go on the Internet and it’s like, if the levels are like this, you know he’ll become retarded. He’s losing IQ points by the second. And I’m like, oh, my gosh! I’m looking at him, and like, he seems fine. Is his brain, you know, getting destroyed by the protein that’s in my breast milk? PATIENT IN WAITING: TESTING Vague symptoms No advance warning Prenatal testing Parents visit metabolic clinic Captive audience motivated by fear-anxiety Continued contradictory messages mixed with uncertainty HYPERPROLINEMIA "The ultimate way of figuring this out would be to test the genes. Those tests are not available clinically. They are available on a research basis.” Can symptoms appear late in life? "They could. We don't know. I can't guarantee anything but the fact that she is developmentally perfectly on target is a good sign." The foster mother asks about warning signs besides seizures. The physician explains that they should be attuned to regular developmental landmarks such as sitting, walking, and babbling in time. PATIENT-IN-WAITING: TESTING No answers to questions Is hyperprolinemia a true disease? Sequence of testing Unavailable or inconclusive Developmental markers EVEN WITH “CONCLUSIVE” TEST, NO ENDPOINT MCADD: two common mutations Possibility: classic and unknown mutation “She still has MCADD and we’ll need to treat her as if she does—if she did go in metabolic crisis or if she was vomiting or had diarrhea you still need to do the same as if she had a severe case of MCADD. So he didn’t ever say, 'She doesn’t have it anymore.” PATIENT-IN-WAITING Preventive measures receive traction in life Paperwork confirms diagnosis Families organize around diagnosis HYPERPROLINEMIA "We were not sure whether it was simply a delay where it would soon happen or there was something that is going on inside." physical and occupational therapy. The "diagnosis" of hyperprolinemia has had consequences in the adoption process. PATIENTS-IN-WAITING no conclusive ending: fading away Genetics team: nothing has changed so things are probably well The child is "not sick but he's not normal." Parents: nothing has changed so we are still in danger Safety due to preventive measures Exceptions: some Spanish speaking families, family suspicious of experimentation DOES NEWBORN SCREENING SAVE LIVES? Not an epidemiological answer Four possible outcomes: Child does well in spite of NBS Patients-in-waiting Maternal disease Child does poorly in spite of NBS 11 kids with severe developmental delay 3 children died Other studies: including MCADD Child does poorly due to NBS Overtreatment Misdiagnosis Child does well due to NBS WHAT DOES IT MEAN “CHILD DOES WELL DUE TO NEWBORN SCREENING?” Window of opportunity MCADD: swine flu Geneticist: “The most important thing is when they get sick, get them to a hospital, and make sure that they are eating. If they eat, they’re protected. Although people talk about low-fat diets, talk about carnitine, the essential treatment is just not letting them become ill. With this condition, it’s easy to treat, so that unless you live in the middle of nowhere—” Mother: “Or getting to the emergency room. Or have a doctor that will take you seriously. Or have a rapid onset disorder. You make it sound like it’s so easy: like all you do is get them to the ER. So much happens before they get sick, and before you get to a [IV] drip.” Presumes connecting gaps: transportation, time, communication skills, organize life around possibility of crisis Articulation work: someone needs to step up to the plate. HEALTH SERVICE BARRIERS Health Insurance: free screening but pay for follow-up Public insurance program: covered if included in contract HMO: covered if authorization Co-pay Refuse authorization Maternal disease not covered Medical foods and supplements PKU coverage is state mandated Others depend: requires authorization Therapeutic services Early Start: up to 3 years Afterwards: school or regional center Transportation Language CONCLUSION Social consequences of genetic screening “New” patient population Diagnostic odyssey Results confirmed by DeLuca, Kearney, Norton, Arnold in Pediatrics Universality of newborn screening Window of opportunity to saving lives Disease not amenable to prevention Highest priority dedication from parents Systematic inequity problems It takes a village … THANK YOU