Chapter 18
Liver and Biliary Tract
The liver
Normal adult liver weighs 1400-2600 gm
2.5% of body weight
Dual blood supply
The portal vein -60-70%
The hepatic artery – 30-40%
The porta hepatis- hilum – transverse fissure in the inferior
surface
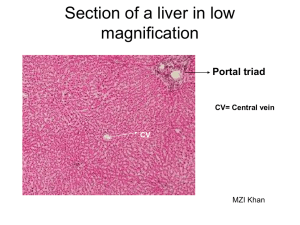
Portal tracts- portal veins, hepatic arteries, bile ducts
The liver
Hepatic microarchitecture
Lobular model
1-2mm hexagonal lobules oriented around the terminal tributaries of the hepatic vein with portal tracts at the
Centrilobular
Periportal
Acinar model
Hepatocytes near terminal hepatic veins are apices
Penetrating septal venules from the portal vein are the bases
Triangle with 3 zones
Zone 1 closest to the blood supply
Zonation of the parenchyma is important
Gradient of activity displayed by many hepatic enzymes
Zonal distribution of certain types of hepatic injuries
Hepatocytes arranged in sheets
Sinusoids between the sheets
most richly perfused cells in the body
discontinuous endothelial cells
space of Disse
Kuppler cells
Hepatic stellate cells
bile canaliculi canals of Hering bile ductulesterminal bile ducts
lymphocytes
periphery
General Features of Hepatic diseases
Major primary diseases of the liver
Viral hepatitis
Alcoholic liver disease
Nonalcoholic fatty liver disease
Hepatocellular carcinoma
With the rare exception of fulminant hepatic failure, liver disease
is insidious, enormous functional reserve
Newly diagnosed chronic liver disease -72/100,000
1.1% of al deaths in the US
Laboratory evaluation of liver disease
Hepatocyte integrity
AST
ALT
LDH
Biliary excretory function
bilirubin – total, direct, delta
urine bilirubun
bile salts
AP
GGTP
5”-nucleotidase
Hepatocyte function
Albumin
PT
Ammonia
aminopyrine breath test
galactose elimination
Patterns of liver Injury
Hepatocyte degeneration and intracellular accumulations
Hepatocyte necrosis
Inflammation
Regeneration
Fibrosis
Syndromes
Hepatic failure
Cirrhosis
Portal hypertension
Disturbances of bilirubin metabolism
jaundice, cholestasis
Hepatic failure
Acute liver failure
associated with encephalopathy within 6 months of diagnosis
massive hepatic necrosis
drugs or toxins
In US
50% acetaminophen
14% other toxins including
mushrooms
4% hepatitis A
8% hepatitis B
15% autoimmune and unknown
Chronic liver disease – cirrhosis
Hepatic dysfunction without overt necrosis tetracyline, acute fatty liver of
pregnancy
Hepatic Failure
Clinical features
jaundice
hypoalbuminemia peripheral edema
hyperammonemiacerebral dysfunction
fetor hepaticus portosystemic shunting
impaired estrogen metabolism
palmar erythema
spider angiomas
Males – hypogonadism, gynecomastia
Coagulopathy
Hepatic encephalopathy
Spectrum of disturbances in consciousness
Rigidity, hyper-reflexia, asterixis
Disorder of neurotransmission in the CNS and
neuromuscular system
Minor morphologic changes in the brain
Reversible
Associated with elevated ammonia levels
Hepatorenal syndrome
Appearance of renal failure in patients with
severe chronic liver disease
8% per year among patients with cirrhosis and
ascites
Precipitating stress factor
Poor prognosis
Hepatopulmonary syndrome
Triad – chronic liver disease, hypoxemia,
intrapulmonary vascular dilations
Enhanced production of NO by the lung key
mediator
Respond to O2
Diffusion-perfusion defect
Cirrhosis
Chief worldwide causes
Alcohol abuse
Viral hepatitis
NASH ( non-alcoholic steatohepatitis)
Three main morphologic characteristics
Bridging fibrous septa
Parenchymal nodules
Disruption of the architecture of the entire liver
Cirrhosis
Pathogenesis
death of hepatocytes
extracellular matrix deposition
vascular reorganization
Predominant mechanism of fibrosis
proliferation of the hepatic stellate cell
activation of these cells into highly fibrogenic cells
Shunting of blood from the parenchyma
Loss of fenestration of the sinusoidal endothelial cells
Stimulus for hepatic stellate cell proliferation
chronic inflammation
cytokine and chemokine production by Kuppler cells, endothelial cells,hepatocytes, and bile dust endothelial cells
disruption of the ECM
direct stimulation of the stellate cell by toxins
Surviving hepatocytes stimulated to regenerate as nodules
Result is a fibortic nodular liver
delivery of blood to the hepatocytes is compromised
ability of hepatocytes to secrete substances into the plasma is compromised
Biliary channels are obliterated
Clinical features
Nonspecific- anorexia, weight loss, weakness,
Then signs of hepatic failure
Mechanism of death in most
progressive liver failure
complication related to portal hypertension
development of hepatocellular carcinoma
Portal hypertension
Prehepatic
obstructive thrombosis
narrowing of the portal vein
massive splenomegaly
Intrahepatic
cirrhosis
Posthepatic
severe right-sided heart failure
constrictive pericarditis
hepatic vein outflow obstruction
Portal hypertension
Pathophysiology
Increased resistance to flow at the level of the sinusoids
Increase in portal venous blood flow resulting from a hyperdynamic circulation
arterial vasodilation
Role of NO
Major clinical consequences
ascites
formation of portosytemic venous shunts
congestive splenomegaly
hepatic encephalopathy
Pathogenesis of the ascites
Sinusoidal hypertension
percolation of hepatic lymph into the peritoneal cavity
splanchnic vasodilation and hyperdynamic circulation
Portosystemic shunts
rise in portal system pressure reversed flow from portal to systemic circulation
venous bypasses
hemorrhoids
esophageal varices*** massive hematemesis and death
retroperitoneum
falciform ligament of the liver (periumbilical and abdominal wall)
caput medusae* hallmark of portal hypertension
Splenomegaly
massive congestion
secondary thrombocytopenia or pancytopenia
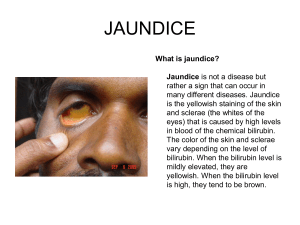
Jaundice and Cholestasis
Common causes of jaundice
bilirubin overproduction
hepatitis
obstruction of the flow of bile
Two major functions of bile
emulsification of dietary fat in the lumen of the gut through the detergent action of bile salts
elimination of bilirubin, excess cholesterol, xenobiotics and other waste products that are not
water-soluble enough to be eliminated by the kidney
Metabolism of bilirubin
uptake from the circulation
intracellular storage
conjugation with glucoronic acid
biliary excretion
Bilirubin and bile formation
Bilirubin is the end-product of heme degradation
Heme to biliverdin via heme oxygenase
Biliverdin to bilirubin via biliverdin reductase
Bound to albumin and transported to the liver
Uptake by the hepatocytes and conjugated by
UDP-glucuronic transferase
Excreted into the bile
Deconjugated in the bowel by bacteria to urobilinogens and excreted in the
feces
Enterohepatic circulation
Bile acids in bile salts are highly effective detergents for lipids secreted by the
hepatocytes into the bile and dietary lipids in the bowel lumen
Pathophysiology of Jaundice
Unconjugated bilirubin is virtually insoluble in
water at physiologic pH and exists in tight
complexes with albumin
A very small amount exists as albumin-free
anion in plasma – can increase if becomes
unbound from albumin by protein-binding
drugs or in severe hemolytic disease can
diffuse into tissues - kernicterus
Pathophysiology of jaundice
Conjugated bilirubin is soluble,non-toxic and
only loosely bound to albumin
Exess can be excreted in the urine
Delta bilirubin is covalently bound to albumin if
there is prolonged elevated conjugated
hyperbilirubinemia
Pathophysiology of jaundice
Jaundice occurs when the equilibrium between bilirubin
production and clearance is disturbed by:
Unconjugated
Excessive extrahepatic production
Reduced hepatocyte uptake
Impaired conjugation
Conjugated
Decreased hepatocellular excretion
Impaired bile flow
Causes of jaundice
Unconjugated
Excess production
Hemolytic anemias
Resorption of blood from internal hemorrhage
Ineffective erthropoiesis
Reduced hepatic uptake
Drug interference with membrane carrier system
Some cases of Gilbert syndrome
Impaired bilirubin conjugation
Physiologic jaundice of the newborn
Breast milk jaundice
Genetic deficiency of UGT1A1 activity
Gilbert syndrome
Diffuse hepatocellular disease
Conjugated
Deficiency of canalicular membrane transporters
impaired bile flow
Hereditary Hyperbilirubinemias
Unconjugated
Crigler-Najjar syndrome
Type I
Type II
Gilbert syndrome
Conjugated
Dubin-Johnson syndrome
Rotor syndrome
Cholestasis
Impaired bile formation and flow
Accumulation of bile pigment in the hepatic parenchyma feathery degenerationbile lakes
Extra hepatic or intrahepatic obstruction of bile channels
Defects in hepatocyte bile secretion
Clinical
jaundice, pruritus, skin xanthomas, malabsorption, fat-soluble
vitamin deficiency
elevated AP, GGTP
Progressive Familial Intrahepatic Cholestasis
PFIC -1,2,3
Infectious disorders
Viral hepatitis
A,B,C,D,E,G
HAV
benign, self-limited disease
incubation 3-6 weeks
ssRNA
never causes chronic liver disease
sporadic febrile disease
Vaccine available
Viral hepatitis
HBV
Acute hepatitis with recovery
nonprogressive chronic hepatitis
progressive chronic disease ending in cirrhosis
fulminant hepatitis with massive liver necrosis
asymptomatic carrier state
10% chronic liver disease
partiallly dsDNA
Vaccine available
incubation 1-4 months
highest carrier rate is in perinatally acquired infection
HBV genome codes for
core protein
envelope gycloproteins
polymerase
HBx
HBsAg
Anti-HBs
HBeAg
HBV-DNA
DNA polymerase
anti –HBc
the host immune response is the prime determinant of the outcome of infection
Viral Hepatitis
HCV
the most common chronic blood-borne infection
ssRNA
incubation 7-8 weeks
80% chronic liver disease
most common cause of chronic liver disease in the US and the most common reason for liver transplant
Risk factors
IV drug use (54%)
multiple sex partners
surgery within last 6 months
needle stick injury
multiple contacts with HCV-infected person
employment in medical or dental field
unknown (32%)
inherently unstable, multiple genotypes and subtypes, quasispecies
hampered vaccine efforts
elevated titers of anti-HCV IgG occurring after an active infection do not consistently confer effective immunity
Characteristic feature of HCV infection is repeated bouts of hepatic damage, the result of reactivation of a preexisting
infection or emergence of an endogenous, newly mutated strain
85% acute infection is asymptomatic
HCV RNA to assess viral replication
Viral hepatitis
HDV
Circular defective ssRNA
dependent on HBV for its life cycle
Acute coinfection with HBV established first
Superinfection of chronic carrier
Helper-dependent latent infection in liver
transplant setting
Viral hepatitis
HEV
ssRNA
incubation 4-5 weeks
No chronic liver disease
fecal-oral
zoonotic
high mortality rate in pregnant woman – 20%
Viral hepatitis
HGV
not hepatotropic
bone marrow and spleen
no human disease
somewhat protective against HIV disease if
coinfecting a HIV+ person
Viral hepatitis
Clinicopathologic Syndromes
Acute asymptomatic hepatitis with recovery ( serologic evidence only)
Acute symptomatic hepatitis with recovery ( anicteric or icteric)
Chronic hepatitis with or without progression to cirrhosis
Fulminant hepatitis with massive to submassive hepatic necrosis
Carrier state
Viral hepatitis
Acute
Ballooning degeneration
macrophage aggregates
apoptosis
bridging necrosis
Kuppler cell hypertrophy and hyperplasia
portal tract infiltration with inflammatory cells
interface hepatitis
ductular reaction
Viral hepatitis
Chronic
smoldering hepatocyte apoptosis
lymphoid aggreagtes
bile duct reactive changes
macrovesicular steatosis
interface hepatotis
bridging necrosis
deposition of fibrous tissue
Other liver infections
Toxic shock – Staph.aureus
Typhoid fever – Salmonella typhi
Syphilis – T.pallidum
Ascending cholangitis
Parasitic – malaria,schistosomiasis, strpngtloidiasis, cryptosporidosis, leishmaniasis,
echinococcosis, liver flukes
Abscesses
Developing countries – echinococcal and
amebic
Developed countries – pyogenic
portal vein
arterial supply
ascending from then biliary tract
direct invasion from nearby source
penetrating injury
Fever, RUQ pain, tender hepatomegaly, jaundice
Autoimmune hepatitis
Unknown etiology
Chronic and progressive
Triggers – viral infections, drugs, herbal products
Conurrently with other autoimmune disorders
Female predominance
Clusters of plasma cells in the interface of portal tracts and
hepatic lobules
Type 1 – ANA, SMA, AAA Anti-SLA/LP
Type 2 – ALKM-1, ACL-1
Treatment – immunosuppressives, transplant – can recur in
transplanted livers
Drug and Toxin-Induced Liver
disease
Drug-induced liver injury
10% of adverse drug reactions
most common cause of fulminant hepatitis in US
Injury from:
direct toxicity
hepatic conversion of xenobiotic to an active toxin
immune mechanisms
Predictable(intrinsic) or unpreditable(idiosyncratic)
Reye syndrome
Exposure to a toxin or therapeutic agent should always be
included un the differential diagnosis of liver disease
Alcoholic liver Disease
Three forms
Hepatic steatosis-reversible if abstention from further alcohol
shunting away from catabolism to lipid biosynthesis
impairedassembly and secretion of lipoproteins,
inreased perioheral catabolism of fat
Alcoholic hepatitis-hepatocyte swelling and necrosis, Mallory bodies, neutrophilic reaction, fibrosis
acealdehyde
Cytochrome P-450 active oxygen species
oxidative injury
malnutrition and vitamin deficiencies
release of bacterial endotoxin from the gut inflammatory response
release of endothelins from sinusoidal endothelial cells decrease in sinusoidal perfusion
Cirrhosis
Pathogenesis
Gender, ethnic, genetic, comorbid conditions
Steatosis, dysfunction of mitochondrial and cellular
membranes, hypoxia, oxidative stress
Metabolic Liver Disease
NAFLD
Hepatic steatosis
Steatosis accompanied by minor, non-specific
inflammation
NASH
Most common cause of chronic liver disease in
the US
Obesity and metabolic syndrome
Hemachromatosis
Excessive accumulation of iron
Abnormal regulation of intestinal absorption of dietary iron
Micronodular cirrhosis
Diabetes mellitus
Skin pigmentation
AR
Slow progression – 5-6th decade
Men> women
HFE- adult form
HJV- juvenile form
Deposition of hemosiderin in liver, pancreas,myocardium, oituitary, adrenal, thyroid and parathyroid, joints,skin
Cirrhosis
Pancreatic fibrosis
Clinical – hepatomegaly, abdominal pain,skin pigmentation,diabetes, ardiac dysfunction,arthritis,
hypogonadism
200-fold increase risk of hepatocellular carcinoma – treatment for iron overload does not remove the risk
Removal of excess iron can reverse the toxic changes if cells are not fatally injured
Neonatal hemochromatosis
Not inherited
Unknown etiology
No treatment
Damage begins in utero
Hemosiderosis ( secondary
hemochromatosis)
Parenteral iron overload
Ineffective erythropoiesis withincreased
erythroid activity
Increased oral intake of iron- Bantu siderosis
Congenital atransferrinemia
Chronic liver disease
Wilson disease
AR
Impaired copper excretion into the bile
Failure to incorporate copper into ceruloplasmin
Toxic levels of copper in brain, liver, eye
Kayser-Fleisher rings
Clinical- 6-40 years of age
Acute or chroni liver disease, neuropsychiatric manifestations,
tremor
Decrease in serum ceruloplasmin, inrease in liver copper,
increased urinary secretion of copper
Chelation therapy or zinc-based therapy very sucessful if
recognized early
Alpha 1-Antitrypsin deficiency
AR
Major function of this protein is the inhibition of
proteases released from neutrophils
Without it pulmonary emphysema and liver disease
develop
Cutaneous panniculitis, arterial aneurysm,
bronchiectasis, Wegener’s granulomatosis
Neonatal hepatitis with cholestatic jaundice
in 10-20% of newborns with the deficiency
Neonatal Cholestasis
1/2500 live births
Prolonged conjugated hyperbilirubinemia
Cholangiopathies (primarily biliary atresia)
Neonatal hepatitis
Major causes
Bile duct obstruction
neonatal infection
toxic
metabolic disease
miscellaneous
idiopathic
Imporant to differentiate biliary atresia( needing surgical intervention)
Biopsy shows multinucleated giant hepatocytes in neonatal hepatitis
Intrahepatic Biliary Tract disease
Secondary Biliary cirrhosis
Prolonged obstruction of the biliary tree
Gallstones or malignancy or strictures
in children
biliary atresia
CF
choledochal cysts
pauity of bile ducts (Alagille)
proliferation of smaller bile ductules
bile lakes
feathery degeneration
ascending infections – Gram- enteric organisms
Intrahepatic Biliary tract disease
Primary Biliary cirrhosis
nonsuppurative, inflammatory destruction of medium-sized intrahepatic bile ducts
Autoimmune?
antimitochondrial antibodies
females> males 6:1
fatigue, pruritus, hepatomegaly,
hyperpigmentation, eyelid
xanthelasmas,arthropathy
Small-duct biliary fibrosis and cirrhosis
dense accumulation of lymphocytes,macrophages,plasma cells, and occasional eosinophils
Extrahepatic manifestations of autoimmunity
Sjogren syndrome, systemic sclerosis, thyroiditis, RA, Raynaud’s,
membranous GN,
celiac disease
Treatment with ursodeoxycholic acid – mechanism of action?, remission and prolonged survival in 25-30%
5
Intrahepatic BiliaryTract disease
Primary Sclerosing cholangitis
Inflammation and obliterative fibrosis of
intrahepatic and extrahepatic bile ducts, with
dilation of preserved segments
Associated with IBD
Cholangiocarcinoma
Anomalies of the biliary trees
Von Meyenburg Complexes
bile duct hamartomas
Polycystic liver disease
Congenital hepatic fibrosis
Caroli Disease
All of the above can be associated with polycystic kidney disease
Alagille Syndrome (paucity of bile ducts)
AD
chronic cholestasis, peripheral stenosis of the pulmonary artery,
butterfly-like vertebral arch defects, posterior embryotoxon (eye defect)
hypertelic facies
Circulatory disorders
Impaired blood inflow
hepatic artery compromise
portal vein obstruction-umbilical catheter, intra-abdominal sepsis,hypercoagulable disorders,
trauma, pancreatitis, HCC, pancreatic cancer, cirrhosis
Intra- or extrahepatic thrombosis
Impaired intrahepatic blood flow
cirrhosis
sinusoid occlusion
systemic circulatory compromise – nutmeg liver – centrilobular hemorrhagic necrosis
Hepatic vein outflow obstruction
Hepatic vein thrombosis ( Budd-Chiari)
sinsoidal obstructive syndrome- Jamaican bush teadrinkers, allogeneic marrow transplants
Hepatic complications of organ or
bone marrow transplantation
Graft-versus-host and liver rejection
Endothelitis – subendothelial lymphocyte
proliferation lifts the endothelium away from
the basement membrane
Hepatic disease associated with
prenancy
HEV infection more severe in pregnant woman – 10-20% mortality
Preeclampsia and eclampsia
maternal hypertension
proteinuria
peripheral edema
coagulation abnormalities
DIC
HELLP syndrome – hemolysis, elevated liver enzymes, low platelets
Hyper-reflexia and seizures+eclampsia
hemorrhage into the space of Disse, hepatic hematoma, dissection of blood under
Glisson’s capsule leading to hepatic rupture
Acute fatty liver of pregnancy (AFLP)- mitochondrial dysfunction
Interhepatic cholestasis of pregnancy- pruritus
Nodular hyperplasias
Focal nodular hyperplasia
Nodular regenerative hyperplasia
Alterations in blood supply
Obliteration of portal vein radicles and
compensatory augmentation of arterial blood
supply
Benign neoplasms
Cavernous hemangiomas
most commn benign liver tumor
Hepatic adenomas
young women on oral contraceptives
May be mistaken for malignant HCC
subcapsular can rupture and cause intraperitoneal
hemorrhage
Transform to malignant – glycogen storage disease
No portal tracts
Malignant Tumors
Angiosarcomas- vinyl cholorde, arsenic,
Thorotrast
Hepatoblastoma- epithelial or epithelialmesencymal, familial adenomatous polyposis,
Beckwith-Wiedmann
HCC
Cholangiocarcinoma
Hepatocellular carcinoma
Third most frequent cause of cancers deaths
Chronic viral infection
Chronic alcoholism
NASH
Food contaminants
Tyrosinemia -40% develop the tumor
Repaeted cycles of cell death and regeneration
Strong propensity for invasion of vascular structures
Unifocal, multifocal, diffusely infiltrative
Fibrolamellar carcinoma – young adults, usually no underlying chronic liver
disease
Alpha feto-protein levels
Death due to cachexia, GI bleeding, liver failure with coma,rupture of the
tumor
Cholangiocarcinoma (CCA)
Malignancy of the biliary tract
Liver fluke
Klatskin tumors –perihilar, junction of right and
left hepatic ducts
Periampullary carcinoma – along with
adenocarcinomas of the duodenum and
pancreatic carcinoma
Metastatic tumors
More common than primary liver cancers
Most common – colon, breast, lung, pancreas
Amazing amount of involvement before
laboratory evidence of hepatic dysfunction
The Biliary Tract
95% of biliary disease is attributable tp
cholelithiasis ( gallstones)
1 liter of bile is secreted by the liver each day
Gallbladder has the capacity 0f 50 ml
Not essential for biliary function
Congenital anomalies
Absent
Duplication
Bilobed
Aberrant locations
Folded fundus (phrygian cap) – most common
Agenesis of all or any portion of the hepatic
ducts and hypoplastic narrowing of biliary channels (
true biliary atresia)
Disorders of the gall bladder
Cholelithiasis
vast majority are silent
Two main types
cholesterol -90%
pigment stones ( bilirubin calcium
salts)
Risk factors for gallstones
Cholesterol stones
Demography- northern Europeans, N and S Americans ,
Native Americans
advancing age
Female sex hormones
obesity and metabolic syndrome
rapid weight reduction
gallbladder stasis
inborn errors of bile acid metabolism
hyperlipidemia syndromes
Pigment stones
Demography – Asians, rural
Chronic hemolytic syndromes
bilary infection
GI disorders
Four contributiong factors for
cholelithiasis
Supersaturation
Gallbladder hypomotility
Crystal nucleation
Accretion within the gallbladder mucous layer
Clinical features
10-20% cholesterol stones are radio opaque
50-75% pig,emt stones are radioopaque
70-80% aymptomatic
Biliary pain – excruciating and constant or “colicky”
Complications – empyema, perforation, fistulas,
inflammation, obstructive cholestasis or pancreatitis,
gallstone ileus (Bouveret’s syndrome), increased risk
for carcinoma
Cholecystitis
Acute calculous
inflammation precipitated 90% of the time by obstruction of the neck or cystic duct
chemical irritation
disruption of the mucous layer
dysmotility
compromised blood flow
then later bacterial contamination
Acute acalculous
ischemia
risk factors – sepsis with shock, immunosuppression, major trauma and burns, DM, infections
Clinical features- calculous
RUQ or epigastric pain
Fever, anorexia, tachycardia, sweating, nausea, vomiting
jaundice=obstruction of the common bile duct
leukocytosis, increased AP
Symptoms may appear with remarkable suddenness
Acalculous more insidious
Chronic cholecystitis
Supersaturation of bile predisposes to inflammation as
well as stone formation
Fibrous adhesions, variable degrees of inflammation,
Rokitansky-Aschoff sinuses ( outpouchings of the
mucosal epithelium through the wall), porcelain
gallbladder, xanthogranulomatous cholecystitis,
hydrops of the gallbladder
Recurrent attacks of pain, N, V, and intolerance for fatty
foods
Complications
Bacterial superinfection with cholangitis or sepsis
Gallbladder perforation and local abscess formation
Gallbladder rupture with diffuse peritonitis
Biliary enteric fistula
Aggravation of preexisting medical illness
Porcelain gallbladder with increased risk of cancer
Disorders of the Extrahepatic Bile
Ducts
Choledocholithiasis – presence of stones within the bile
ducts of the biliary tree
aymptomatic, obstruction,pancreatitis, holangitis,
hepatic abscess, secondary biliary cirrhosis, acute
calulous cholecystitis
Cholangitis – bacterial infection of the bile ducts.
Sphincter of Oddi entry point,
Ascending cholangitis –infection of the hepatic biliary
radicles
Biliary atresia
Complete or partial obstruction of the lumen of the extrahepatic biliary tree within
three months of life
1:12,000 live births
1/3 neonatal cholestasis
Progressive inflammation and fibrosis of the intra and extrahepatic bile ducts
Single most frequent cause of death in early childhood from liver disease
Two forms
fetal -20%, other anomalies
perinatal – presumed normal tract is destroyed following birth, viral, autpimmune,
repvirus, rotovirus, CMV
Kasai procedure for type I ( common duct) or Type II (hepatic bile ducts)
90% type III – obstruction at or above the porta hepatis
Choledocal Cysts
Congenital dilation of the common bile duct
Tumors
Adenomas
Inflammatory polyps
Adenomyosis
Carcinoma of the gallbladder
Carcinogenic derivatives of bile acids?