Gram (-) Bacteria:
Neisseria, Enterobacteriaceae, etc.
Nestor T. Hilvano, M.D., M.P.H.
Images Copyright by Bauman, Robert. 2009. Microbiology, With
Diseases by Taxonomy, 3rd edition, Pearson Benjamin Cummings
Learning Objectives
1.
2.
3.
4.
List features of Neisseria that contribute to its pathogenicity.
Compare and contrast the symptoms of gonorrhea in men and women.
Discuss the epidemiology of meningococcal diseases.
Describe diagnostic methods, treatment, and prevention of diseases of
enteric bacteria.
5. Describe the pathogenesis and diseases of Escherichia coli O157:H7.
6. Differentiate between coliform and non-coliform opportunists.
7. Describe the diseases caused by non-coliform opportunistic enteric
bacteria.
8. Describe the diseases caused by truly pathogenic enteric bacteria.
9. Contrast salmonellosis and shigellosis.
10.Identify and describe three diseases caused by species of Haemophilus .
11.Identify the three disease phases of pertussis.
12.Describe Pseudomonas aeruginosa as an opportunistic pathogen of burn
victims and cystic fibrosis patients.
13. Describe the modes of transmission of tularemia.
14.Describe symptoms and treatment of Legionnaires disease.
15.Describe the mode of transmission of Q fever.
Neisseria gonorrhoeae
• Isolated in 1879 by Albert Neisser
• Gram (-), diplococci; aerobic;
oxidase positive
• Fimbriae; antiphagocytic capsule;
CW antigen lipo-oligosaccharide,
composed of lipid A of
lipopolysaccharide (endotoxin)
• Pathogenicity – transmitted by sex;
adhere to mucous membranes, multiply,
invade deeper tissue, and spread (PID)
• Increased vaginal (greenish-yellow
or whitish) discharge, painful
urination – in women
• Dx – organisms isolated; pus
• Rx – cephalosporins or quinolones
Neisseria meningitidis
• Gram (-), diplococci
• Antiphagocytic capsule
• Endotoxin – damages
endothelial cells,
petechial hemorrhages
• Tumbler test for
petechial hemorrhages =
pressed firmly against a
septicemic rash, the
marks will not fade
• Role in bacterial
meningitis
Neisseria meningitidis
• Pathogenesis - spread via respiratory droplets/body fluids
(kissing, sneezing, coughing); present in 4 to 5% (up to
40%) in closed quarters; low immunity for children < 10 y/o
• most common cause of meningitis in children and adults
under 20 of age.
• Stages:
a) 1st stage – mild nasopharyngitis
b) 2nd stage – via lymph to blood →bacteremia =
meningococcemia; fever, malaise, petechial hemorrhages
(spotted fever)
c) 3rd stage – meningitis (1 to 30/10,000), fatal in 6 to 8 hrs.,
mortality of 35 to 80%, s/sx include headache, stiff neck,
vomiting, confusion, delirium
• Dx – spinal tap, blood sample, skin lesions, nasopharynx;
antibody test
• Rx – IV penicillin for patient; prophylaxis for close contacts
Gram (-), Facultative Anaerobic Bacilli
1. Enterobacteriaceae
• Enteric bacteria; intestinal microbiota
• Soil, water, and decaying vegetations
• Ferment glucose anaerobically; reduce nitrate to nitrite
• Lipopolysaccharide – virulence
• Pathogenic enteric bacteria include
1. coliform opportunists – E. coli; K. pneumonia; Serratia;
Enterobacter, Hafnia, and Citrobacter are nosocomial
opportunists
2. non-coliform opportunists – Proteus; Morganella;
Providencia; Edwardsiella
3. true pathogens – Salmonella; Shigella; Yersinia
2. Pasteurellaceae
• Oxidase (+), small,nonmotile, requires heme or
cytochromes
• Pasteurella multicida; Haemophilus influenza
Escherichia coli
• Most common coliform; food – water
borne diseases
• Fimbriae for attachment
• Strains
- enterotoxigenic = enterotoxin +
endotoxin → traveller’s diarrhea
- enteroinvasive = invasion of
intestinal wall → inflammation, fever,
diarrhea, dysentery
- enterohemorrhagic = E. coli
0157:H7; epidemic seen with
undercooked meat or unpasteurized
milk/juice
* O polysaccharide 157
* flagellar H7 antigen
* bloody diarrhea; hemorrhagic
colitis
* hemolytic uremia syndrome
McConkey agar = selective for gm. –
E. coli and differentiates lactose
Fermenting E. coli (red to pink colonies)
Klebsiella pneumonia
• Digestive and respiratory
system
• Capsule = mucoid
appearance and protects
from phagocytosis
• Pneumonia - bloody sputum;
alcoholics and
immunocompromised at
higher risk
• Bacteremia, meningitis,
wound infection, and UTI
Salmonella
• Gm (-); peritrichous bacilli
• Lives in intestines and eliminated in feces
• Enteric fever
a) Typhoid fever – S. typhi; Rx- antibiotics (ampicillin)
b) Paratyphoid fever – S. paratyphi; milder disease
* Pathogenesis – fecal-oral route from contaminated water,
food, drink, and carrier; into lymphatics, RES (liver, spleen,
BM); bloodstream
* Endotoxemia → fever, headache, weakness, diarrhea
and rose spots on abdomen
• Gastroenteritis and dysentery
- Salmonellosis – S. typhimurium; S. enteritidis
- generally no bacteremia or septicimia; not invasive
- Pathogenesis – from meat, milk, eggs, chicken, fish
- GI infection after 12 – 48 hrs. with nausea, vomiting, abdominal pain,
diarrhea (non-bloody), prostration, fever
- Rx: fluid and electrolyte replacement
Shigella
• Gm (-), no flagella, multiply intracellularly
• More prevalent in trophics and subtrophics
• Shigellosis – S. sonnei in U.S.; char. by
abdominal cramps, fever, diarrhea, and purulent
bloody stools (severe form of dysentery)
• Pathogenesis – fecal-oral route; enter the
intestinal epith. cells and multiply; causes
abscess and inflammation of intestinal mucosa;
cause dysentery (loss of fluids/electrolytes)
• Mortality 20%
Yersinia pestis
• virulent, nonenteric pathogen; causes
1. bubonic plague
- bite from infected flea
- high fever; swollen,
painful lymph nodes
(buboes) within a week
- untreated cases lead to
bacteremia and
gangrene, 50% fatal
2. pneumonic plague
- spread from bloodstream into lungs; between
human via airborne
- respiratory distress within 24 hrs.; fatal
Haemophilus influenza
• Gm (-), coccobacillus; oxidase (+)
• Require blood agar
• Found in respiratory flora; transmitted
by droplets (infants & children)
• Polysaccharide capsule - resist phagocytosis
• H. influenza b – most common cause of infantile
meningitis (before immunization; prevented by Hib
vaccine)
• Also causes otitis media, conjunctivitis, sinusitis,
epiglotitis, arthritis, and inflammation of skin
• Rx. – antibiotics (cephalosporins)
• Prev – Hib immunization at 2, 4, 6, 12 months
• H. ducreyi - causes chancroid (soft chancre, painful genital
ulcer); a major co-factor in transmission of HIV
• H. aphrophilus (endocarditis)
Bordetella pertussis
• Obligate aerobe; gm (-), coccobacilli
• Capsule – virulence
• Exotoxin – pertussis toxin, inhibits
ciliary activity
• Endotoxin – cytotoxin, kills epithelium
• Pathogenesis –inhalation of organism,
binding to ciliated epithelium (noninvasive), inhibition of ciliary movement,
inflammation and necrosis of tracheal
epithelium, irritation and cough
• Whooping cough – one of most
frequent/severe disease of infants in
U.S. until immunization in 1940s
Bordetella pertussis
• 3 stages
1˚ stage – catarrhal ; 7-16 days; mild cough to
bad cough (sneezing, malaise, fever)
2˚ stage – paroxysmal; 2-6 weeks; severe cough
with whoop, vomiting, exhaustion, and cyanosis
3˚ stage – convalescence; 3-4 weeks; possible secondary
complication of staph/ streph
• Dx
a. cough on Bordet-Genou agar plate, incubate
and identify organism
b. nasopharyngeal swab, grow on medium cont’g
penicillin
• Rx – antibiotics
• Prev – immunity after convalescence; DPT
vaccine
Pseudomonas aeruginosa
• Gm (-), aerobic bacilli
• Soil, decaying organic matter, moist
environment (pools,sponges,
contact lens solution)
• Fimbriae and capsule – attachment
and resist phagocytosis
• Endotoxin (lipid A) in cell wall
• Exotoxin A and exoenzymes S – inhibit protein synthesis
and contribute to cell death in eukaryotic cells
• Nosocomial infections, common in burn wounds, in lungs
of cystic fibrosis; but can colonize organs and systems
• Pyocyanin discoloration of tissues – indicates massive
infection
• Resistant to wide range of antibiotics
Legionella pneumophila
• Legionellosis (legionnaire’s disease)
• Discovered in 1976
(meeting of Am. Legion in Philadelphia)
• Aerobic, gm (-) bacilli
• From natural waters
• Resistant to chlorine
• Intracellular in amoeba (warm waters, showers,
pools)
• Fever, chills, dry nonproductive cough, headache,
and pneumonia
• Dx – fluorescent antibody or other serologic tests
• Rx – erythromycin
Other Gm (-) Aerobic Bacilli
Bartonella – found in animals
but known to cause human
diseases; bartonellosis;
trench fever;
cat-scratch disease
(localized swelling and tender L.N. in children)
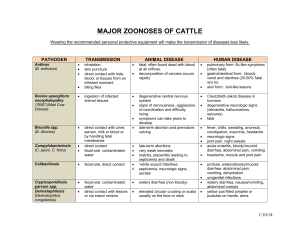
2. Brucella – from unpasteurized contaminated milk or
contaminated animal blood, urine or placentas; brucellosis
(big bang disease and undulant fever), spread to organs,
abortions, granuloma formation, joint pain
3. Francisella – cause zoonotic disease called tularemia
(rabbit fever or tick fever); via biting arthropod or through
unbroken skin
4. Coxiella – C. burnetii, via aerosolized dried feces and urine
of mammals and birds, cause Q fever (fever,headache,
myalgia, and mild pneumonia)
1.
Endotoxin
•
•
•
•
•
Produced by gram – bacteria
Integral part of the cell wall
Lipid A of lipopolysaccharide
Heat stable
Diverse range of host cells and systems
affected
• Diverse range of effects
• Toxoids cannot be made
Homework
1.
2.
3.
4.
5.
Identify causative agent of items listed: petechial hemorrhage in
tumbler test and most common cause of meningitis under 20 of
age; pus urethral discharge in STD; traveler’s diarrhea;
pneumonia in immunocompromised patient; typhoid fever;
shigellosis; buboes; Q fever; tularemia; most common cause of
infantile meningitis; chancroid; legionnaire’s disease; most
common cause of nosocomial infection and in burn infection.
Describe the 3 strains of E. coli as to its toxins.
List microorganisms that cause gastroenteritis (diarrhea and
dysentery) in human.
Discuss the clinical stages of pertussis.
Give the characteristics of endotoxin.