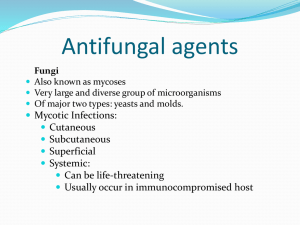
Antifungal Agents
advertisement

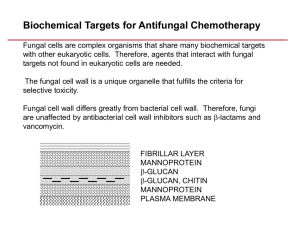
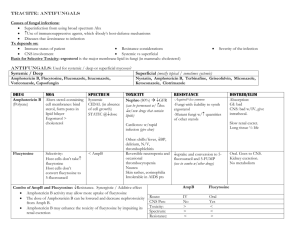
Recommended text books Basic and Clinical pharmacology, 10th or 11th edition, B.G.Katzung, LANGE medical book. Lippincott´s ilustrated reviews: Pharmacology 3rd edition, R.A.Harvey, Champe P.C., R.D. Howland, M.J. Mycek, Lippincott-Raven,. Pharmacology, 6th edition, H.P.Rang, M.M. Dále, J.M. Ritter, Churchill Livingstone, 2007. Antifungal Agents Dr. Roshna S. Aziz Department of Pharmacology School of Medicine University of Sulaimani Widespectrum antibiotics surgery Increase risk Immunosuppressant agents & chemotherapy AIDS FUNGAL INFECTIONS = MYCOSES Opportunistic Systemic or primary or local Slow onset Long duration of therapy Difficult to diagnose & eradicate Symptoms vary from cosmetic to life threatening Antifungal drugs Work by exploiting differences between mammalian and fungal cells to kill the fungal organism without dangerous effects on the host. Both fungi and humans are eukaryots. Difficult to find or design drugs that target fungi without affecting human cells. (side effects) Fungal cell membranes have a unique sterol, ergosterol, which replaces cholesterol found in mammalian cell membranes ANTIFUNGAL DRUGS Systemic & topical some are fungistatic, while others are fungicidal systemic /systemic • Amphotericin B. • Azoles • Flucytosine • Echinocandins Systemic /mucocutaneous • Griseofulvin • Terbinafine Topical /mucocutaneous • Nystatine • Topical Azoles • Topical Allylamines SYSTEMIC ANTIFUNGAL DRUGS FOR SYSTEMIC INFECTIONS AMPHOTERICIN B Broad-spectrum polyene macrolide antibiotic is the most potent antifungal agent for systemic mycosis, in clinical use since 1960 Fungicidal drug at higher concentrations & static at lower levels. Produced by Streptomyses nodosum CSF conc.= 2-3 % of blood conc. Highest concentrations in liver, spleen, bone marrow with less in kidneys and lungs. MECHANISM OF ACTION MECHANISM OF ACTION High affinity for fungal ergosterol, forms “micropore” in fungal cell membrane through which ions, amino acids, & other water soluble substances move out. Markedly increases cell permeability. Cholestrol, present in host cell membranes, closely resembles fungal ergosterol & thus explains the high toxicity of AMB in humans CLINICAL USE Treatment of nearly all life threatening mycotic infections. For systemic disease: slow IV o Local: o Keratitis& corneal ulcers: drops, conjunctival irrigation, o Candiduria: bladder irrigation o Fungal arthritis: local injection SIDE EFFECTS Infusion related Fever & chills, Dyspnea, Nausea &vomiting, Hypotension, Convulsions Cumulative toxicity Nephrotoxicity K & Mg wasting Anemia (↓erythropoietin) To reduce the severity of the infusion-related reactions, pretreatment with an antipyretic (acetaminophen), antihistamines, and antiemetics may be given. Amphotericin B Amphotericin B Liposomal Amphotericin B New lipid formulations Amphotericin B is incorporated into lipid formulations to reduce toxicity & enhance efficacy. This allows higher dose to be used without increasing the toxicity. Much more expensive than ordinary AMB. KEY POINTS AMB is not absorbed enterally; hence can be given orally for intestinal candidiasis. Drug concentration achieved in infected skin is very low, & hence ineffective against superficial fungal infections. Penetration in brain & CSF is poor (but extremely effective in fungal meningitis when combined with 5-FC) FLUCYTOSINE (5-FC) Pyrimidine antimetabolite, narrow-spectrum fungistatic Water soluble • Oral only, Poor protein binding CSF conc. ≈ 75% serum conc. •5-FC (outside) Cytosine permease enzyme •5-FC (inside) •5-FU (inside) Inhibits thymidylate synthase • Inhibits DNA & RNA synthesis Flucytosine is taken up by fungal cells via the enzyme cytosine permease. It is converted intracellularly first to 5-FU and then to 5-fluorodeoxyuridine monophosphate (FdUMP) and fluorouridine triphosphate (FUTP), which inhibit DNA and RNA synthesis, respectively. Human cells are unable to convert the parent drug to its active metabolites. Clinical use at present is confined to combination therapy, either with: Amphotericin B for cryptococcal meningitis , or Itraconazole for chromoblastomycosis ADVERSE EFFECTS • Bone marrow toxicity with anemia, leukopenia, thrombocytopenia, (Mammalian bone marrow cell have the capacity to convert 5-FC to 5-FU) • GI disturbances Mild & reversible liver dysfunction KEY POINTS Since this is a narrow-spectrum fungistatic, it is mainly used as an adjuvant drug & not used as a sole therapy. CSF penetration is excellent, hence it is combined with AMB in fungal meningitis. AZOLES Ketoconazole Imidazoles Miconazole Clotrimazole Azoles Itraconazole Triazoles Fluconazole Voriconazole Posaconazole MECHANISM OF ACTION Inhibition of fungal cytochrome P450 enzymes Reduction of ergosterol synthesis CLINICAL USE BROAD SPECTRUM OF ACTIVITY – Candida, Cryptococcus, Blastomyces, Histoplasma, Coccidiodes , Dermatophytes ADVERSE EFFECTS Relatively nontoxic. Minor GI upset Abnormalities in liver enzymes (inhibit cytochrome P450 enzymes) Very rarely, clinical hepatitis KETOCONAZOLE •(older, more toxic, replaced by itraconazole, but less costly) •The first oral azole introduced into clinical use. •It is less selective for fungal P450 than are the newer azoles. •Absorption variable (better in acidic medium) •Penetration in brain & CSF is poor •In high doses inhibits adrenocortical steroids and testosterone synthesis, resulting in gynecomastia in some males. ITRACONAZOLE •Broad-spectrum antifungal with fungistatic action •MOA: Inhibits fungal ergosterol synthesis like other azoles • Drug absorption is increased by food and by low gastric ph. •Penetration of drug in brain & CSF is poor. • Much more selective than ketoconazole FLUCONAZOLE Broad-spectrum Fungicidal drug; •It is also somewhat effective against some Gram-positive & anaerobic bacteria •Of the orally administered fluconazole 94% is absorbed; •Penetration in brain & CSF is good, hence used for cryptococcal meningitis POSACONAZOLE The newest triazole It is the broadest spectrum member of the azole family. It is the only azole with significant activity against the agents of zygomycosis and mucormycosis. ECHINOCANDINS Caspofungin Micafungin Anidulafungin ECHINOCANDINS The newest class of antifungal . Active against candida and aspergillus, but not c neoformans or the agents of zygomycosis and mucormycosis. MECHANISM OF ACTION Inhibit the synthesis of B glucan in the fungal cell wall Disruption of the fungal cell wall and cell death. ADVERSE EFFECTS Extremely well tolerated, Minor GI side effects Flushing Elevated liver enzymes (caspofungin + cyclosporine). Histamine infusion. release during IV SYSTEMIC ANTIFUNGAL FOR MUCOCUTANEOUS INFECTIONS DRUGS GRISEOFULVIN Very insoluble, fungistatic Derived from a species of penicillium. Better absorption when given with fatty foods. It is deposited in newly forming skin where it binds to keratin, protecting the skin from new infection. Interferes with spindle formation in dividing cells and therefore with mitosis ADVERSE EFFECTS Allergic reaction photosensitivity Hepatitis Teratogenesis TERBINAFINE Synthetic Orally allylamine. Active. Dermatophytoses, especially onychomycosis . Keratophilic , fungicidal. It interferes with ergosterol biosynthesis by: Inhibiting the fungal enzyme squalene epoxidase Accumulation of the sterol squalene, Like the azole drugs, it interferes with ergosterol biosynthesis, but rather than interacting with the P450 system, terbinafine inhibits the fungal enzyme squalene epoxidase. This leads to the accumulation of the sterol squalene, which is toxic to the organism. ADVERSE EFFECTS Rare, mild, self-limiting GI upset Rash Pruritis Headache. Topical antifungal therapy NYSTATIN Only used topically: creams, ointments, suppositories, and other Acts as amphotericin B It is not absorbed , unpleasant taste. Local candidal infections, oropharyngeal thrush, vaginal candidiasis. adverse effects are rare. TOPICAL AZOLES Clotrimazole , Miconazole; Vulvovaginal candidiasis, oral thrush , dermatophytic infections, including tinea corporis, tinea pedis, and tinea cruris. Absorption is negligible, and adverse effects are rare. Topical and shampoo forms of ketoconazole for seborrheic dermatitis and pityriasis versicolor. TOPICAL ALLYLAMINES Terbinafine Both and Naftifine are effective for treatment of tinea cruris and tinea corporis. MOA: Inhibits the squalene epoxidase, leading to accumulation of intrcellular squalene & deficient ergosterol synthesis with subseqent fungal cell death. Terbinafine concentrates in skin and especially at nail beds, making it quite useful for fungal infection of nails Thank you