- A Day of… for GPs
April 4
th
, 2014 – London, ON
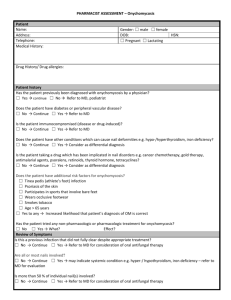
Differential Diagnosis:
The case of the red face
Denise Wexler MD, FRCPC
Top 5 practical tips to take to your clinic tomorrow
1.
2.
4.
5.
3.
Comedones are present in acne
Perioral dermatitis often spares the area just beneath the lower lips
Telangiectasia don't occur in acne or perioral dermatitis
Age of the patient may help in diagnosing a red face
Rosacea often stings or burns
Pediatric and Neonatal Dermatology
Denise Wexler MD, FRCPC
Summary
Classification by morphology is a useful way to organize differential diagnosis
Neonates, especially preterm infants, have thinner skin and are more vulnerable to infection
There are many benign, self limited dermatoses that present in the neonatal period, however careful evaluation is needed to rule out infectious causes, systemic disease, and genodermatoses
Top 5 practical tips to take to your practice tomorrow
1. Erythema toxicum neonatorum is self limiting
2. Milia in infants are self limiting
3. Neonatal herpes simplex is a serious disease and requires systemic treatment
4. Six or more café au lait spots are needed to make a diagnosis of neurofibromatosis
5. Portwine stains in the trigeminial distribution require eye examinations and MRIs
Antibiotic Resistance in Acne
Treatment: Identifying the threat and minimizing risk
Wei Jing Loo MD, FRCPC
Summary Teaching Points
• Pathogenesis of acne vulgaris is the same at all ages, and the
same principles and therapeutic agents apply
• Important considerations for treating younger populations are ease of use (i.e., once daily, combination, etc.), fast onset of action to limit risk of scarring, advanced vehicle to
minimize adverse events on young skin
• Limit the duration and/or use of antibiotics (topical and oral) to reduce the risk of antibiotic resistance (ie. <12 weeks)
Summary Teaching Points
• BPO is an extremely efficacious bactericidal agent for managing acne with anti-inflammatory properties, without the risk of antibiotic resistance
• Retinoid-containing agents are essential for comedonal acne and the prevention of comedonal formation
• Adapalene/BPO is now approved in the U.S. for acne patients
9 years and older
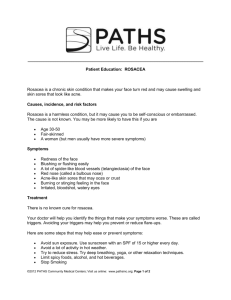
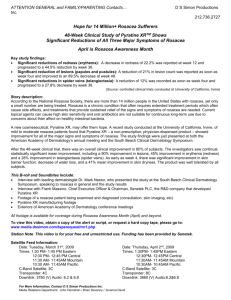
Red and Bumpy: Managing common manifestations of rosacea
Lyn Guenther MD, FRCPC
Rosacea: Conclusions
• Rosacea’s chronic, cyclical inflammatory cycle causes progressive damage to skin structure.
• Early recognition and treatment are important to prevent progression and disfigurement.
• The most common features of rosacea (redness, papules/pustules) require specific individualized management approaches.
Millikan L. The Proposed Inflammatory Treatment Pathophysiology of Rosacea: Implications for Treatment
SKINmed 2(1): 43-47, 2003
Baldwin, H. Diagnosis and Treatment of Rosacea: State of the Art. JDD 2(6):725-730, 2012
Top 5 Practical Tips You can Use in Your
Clinic Tomorrow
1.
Instruct patients to avoid triggers.
2.
Gentle skin care is important.
3.
Chronic therapy is required for continued control.
4.
Sub-antimicrobial oral doxycycline improves rosacea without inducing antibiotic resistance.
5.
Topical Brimonidine can improve facial redness, but may unmask papules, pustules and telangiectasia.
Baseline Hour 3
Diagnosis & Treatment of
Onychomycosis
Denise Wexler MD, FRCPC
Summary – Diagnosis
• Toenail onychomycosis is common and may present as:
– Distal and lateral subungual onychomycosis (DLSO)
– Superficial white onychomycosis (SWO)
– Proximal subungual onychomycosis (PSO)
• Clinical diagnosis should be confirmed by a diagnosis method to identify causative organism and treatment
14
Summary – Treatment Options
• Oral therapies for onychomycosis including terbinafine or itraconazole are recommended:
– Involvement of > 50% of distal nail plate/ multiple nail
• Involvement, involvement of nail matrix
• Transungual therapies for onychomycosis including efinaconazole or ciclopirox are recommended:
– Involvement of < 50%, or when oral therapy is sub-optimal
• Oral and transungual treatment may be combined to improve efficacy and prevent recurrence
15
Summary – Preventing Recurrence
• Recurrence of onychomycosis is frequent and may be due to:
– Poor diagnosis, therapeutic failure, poor prevention
– Patient related factors, such as immunocompromised patients, diabetes etc.
• Maintenance approach is to include:
– Regular follow-up and measures to decrease the risk for reinfection
16
HOT TIPS
1. Ketoconozole should not be used to treat onychomycosis
2. Treatment of onychomycosis requires a positive fungal culture
3. Topical therapy for onychomycosis is safe and efficaceous
4. Efinaconozole topically avoids product build up
5. Long-term topical treatment for onychomycosis may be recommended
17
Moderate to Severe Psoriasis:
What should a GP do?
Lyn Guenther MD, FRCPC
Living Well with Psoriasis – Patient Tools
Summary comments
• Psoriasis is a life-long systemic inflammatory disease
•
Psoriasis has a major impact on quality of life (including work)
• Psoriasis is associated with major co-morbidities (depression, metabolic syndrome, ischemic heart disease, IBD, arthritis)
• Psoriasis treatment options exist for all types and severity levels
• Early initiation of treatment is positively impactful
•
Most patients are managed with topicals
• Adherence is challenging
• Systemic agents may be under-utilized
• A thoughtful review of therapeutic options is ideal
5 Tips to take home
1.
When making the diagnosis of psoriasis, don’t forget to look at the nails, scalp, natal cleft, elbows, knees and sacrum
2.
Check all patients for hypertension, hyperlipidemia, diabetes mellitus and psoriatic arthritis
3.
Treat associated Depression and Anxiety.
4.
Most psoriasis can be controlled/cleared with appropriate therapy, so treat or refer for treatment.
5.
Ask about Adherence at each visit.
Chronic Hand Dermatitis: What is it and how should it be treated?
Lyn Guenther MD, FRCPC
5 tips for Chronic Hand Dermatitis
1.
If possible patch test all patients to identify causative allergens.
2.
If 2 feet, 1 hand involved, do a KOH smear and take a fungal culture to rule out Tinea pedis and manum.
3.
Frequent application of lubricants may prevent fissures.
4.
Ceramide or oat containing lubricants may repair the skin barrier .
5.
Application of nail glue containing Cyanoacrylate can seal fissures and reduce pain.