Staying Afloat, Keeping the Wheels Down and Feet Forward
advertisement

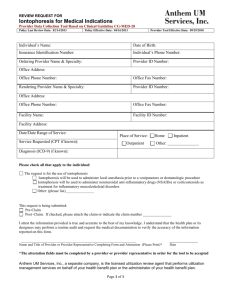
Staying Afloat, Keeping the Wheels Down and Feet Forward Prevention and Management of Repetitive Stress Injuries in the Triathlete Dr. John L. Michie Experience Certified Chiropractic Sports Physician Certified in Physiological Therapeutics Certified Exercise Physiologist Certified in Clinical Nutrition Certified Myofascial Dry Needle Therapist Certified Functional Medicine Practitioner 20 years in clinical practice working w/athletes +2,000 hours of post doctorate education Program Highlights I. II. III. IV. V. VI. Mechanisms of Injury Applied Kinesiology and the Kinetic Chain Connective Tissue Support Managing Inflammation Self Corrective Measures When to Seek Treatment and What Modalities are Best? Common Injuries of the Triathlete Runner’s Knee/Patella Femoral Syndrome/Chondromalacia Achilles Tendonitis Swimmer’s Shoulder IlioTibial Band Friction Syndrome Sciatica (Discogenic and Piriformis) Sacroiliac Syndrome Plantar Fasciitis Common Injuries of the Triathlete Medial Tibial Stress Syndrome Meniscal Tears Adrenal Fatigue Degenerative Disc and Joint Disease Lower Extremity Stress Fractures Rotator Cuff Tendonopathy Ken Hutchins “Exercise is not an Adjunctive Therapy, Exercise is the Therapy.” Mechanisms of Injury Repetitive Stress Trauma Triathlon training consists of massive repetitive stress to multiple body regions!! All endurance training consists of repetitive stress!! In RST, Connective Tissue failure occurs due to excessive loading and/or poor biomechanics Mechanisms of Injury Connective Tissue Tendons connect muscle to bone and transmit mechanical energy Ligaments connect bone to bone - denser and provide some shock absorption Myo-tendinous Junction is a transitional area and highly vulnerable to injury Tendons and Ligaments are largely made up of Collagen Mechanisms of Injury Exhaustive Endurance Training creates damage via metabolic disturbances and ischemia! (Ischemia Induced Muscle Damage) – restoring blood flow critical! Muscle Contusion injuries (Swim?) – may lead to excessive fibroblastic activity and formation of bone within the muscle Mechanisms of Injury Stretch Injuries occur when the movement exceeds the flexibility of the joint/ligament capacity resulting in micro-tears. Biomechanical imbalances are the underlying causes of most soft tissue related injuries! “The Kinetic Chain is integrated and if faults exist anywhere there will be an insidious development of injury at or remote to the fault site!” JLM Inflammation! Cardinal Signs: Heat Swelling Pain Redness Loss of Function Inflammation and Repair Remove inflammatory debris by Phagocytosis Granulation/Scar Tissue Formation Tissue Remodeling ~6 days post injury Collagen is laid down randomly NSAIDs interfere w/collagen formation! Inflammation and Repair! Immobilization of a healing injury compromises strength and collagen orientation Mobilization results in stronger, faster healing of connective tissue injuries!! The greater the amount of injured tissue, the more scar tissue deposition Inflammation and Repair! Ischemia-induced Muscle Injury is caused by damage to vessels seen in endurance sports (Compartment Syndromes) Extent of injury proportional to duration of pressure Nerve injury may result due to persistent pressure Can result in excessive scar tissue formation and cell death Kinetic Chain imbalances lead to over-utilization of muscle groups and this may lead to ischemia Inflammation and Repair! Inflammatory Response & Time Frame of Healing: Acute phase: 24-48 hours Proliferative phase: 3-7 days post injury Repair phase: few days to few weeks Remodeling phase: several months….. Immobilization Negative Effects of Immobilizing Injuries: Cartilage deterioration Bone strength/mass loss Ligament strength and pliability loss Adhesion formation magnified Muscle atrophy Longer rehabilitation windows Treatment Protocols Acute Phase: Goal: Control Pain and Inflammation “PRICE” Protect Rest Ice Compression Elevation Treatment Protocols Physiological Therapeutics: – Ice 30 minutes per application (Avoid Hunter Reaction!) – Electrotherapy (IFC, HV, etc.) – Ultrasound (Pulsed & Continuous) – Iontophoresis – Moist Heat – Post Acute Phase Treatment Protocols Joint Mobilization/Manipulation: – Stimulates mechanoreceptors – Decreases joint congestion – Relieves compressive forces on articular cartilage and structures – Relieves contracture of tissues – Breaks down adhesions – Enhances biomechanical alignment Treatment Protocols Soft Tissue Mobilization and Cross Fiber massage: – Breaks down scar tissue and adhesions – Activates phagocytosis – Creates fiber re-alignment – Accelerates healing and minimizes reoccurrence!! Treatment Protocols Biomechanical Adjustments – Restores optimal kinetic chain alignment – Facilitates biomechanical integration – “Resets” neurological firing patterns – Stimulates healing and joint function – Reduces pain – Minimizes re-occurrence Treatment Protocols Kinesio-taping – Mechanical Correction “Recoiling” – Fascia Correction “Holding” – Space Correction “Lifting” – Ligament/Tendon Correction “Pressure” – Functional Correction “Spring” – Lymphatic Correction “Channeling” Nutritional Management Anti-Inflammatory Protocol: Avoidance of Sugar, Trans Fats, Grains and Dairy (Grain fed animal products + eggs also inflame!) Increase Hydration! Proteolytic Enzymes – 3-6 tid w/o food (Vegetarian and/or Non-Vegetarian) – Trypsin, Chymotrypsin, Bromelain, Papain (Wobenzyme, Protrypsin) Omega 3 Fatty Acids/Fish Oil – 6-9g/day Nutritional Management Ginger, Boswellia, Turmeric (Cox 2 Inhibitors) (Inflavonoid I.C.) CoEnzyme Q10 100-200mg/day Mixed Anti-Oxidants Mixed Bioflavonoids 2-3Kmg/day ALA (Flax), Chia GLA (Borage) Willow Bark Extract Devil’s Claw Extract 30-90 day high dosing for pharmacological effects! Connective Tissue Integrity Nutritional Protocol Amino Acids (Glycine, Proline, Lysine) BCAAs (Leucine, Isoluecine, Valine) Vitamin C Mixed Bioflavonoids Green Lipped Mussels MSM Horsetail Extract (Silica) Hyaluronic Acid Glucosamine/Chondroitin Sulfates Manganese (Collagenics, Ligaplex I and II) Runner’s Knee Causes: Pronation Q-angle (Women > Men) Quadriceps Imbalances/Weakness Tight Hamstrings and ITB Short Hip Flexors Road Pitch Repetition Overly Supportive Training Shoes Wearing Training Shoes beyond ~400 miles Runner’s Knee Symptoms: Pain behind and around the Patella Pain with walking, running, squatting, kneeling Increased pain with downhill running Popping, grinding in and around the knee jt. Runner’s Knee Management: PRICE Acute Physiotherapy protocols (Iontophoresis) Nutritional Anti-inflammatory protocol Strengthen Quadriceps Myofascial release and foam roller @ Hamstrings, ITB, Hip Flexors Orthotics for foot imbalances, pronation, etc. Pool Running Evaluate Shoes for wear patterns, breakdown, etc. Manual manipulation, alignment of kinetic chain imbalances Bracing for Patella stabilization and compression Proprioceptive input training with balance board and bosu ball Achilles Tendonitis Causes: Reduced Flexibility or weakness in Calf Group Overuse or increased training intensity or volume Less recovery time between running sessions Increased hill or speed work!! Unequal leg length Pronation or Supination Ankle or Foot Joint Fixations Poor Heel posting, poor shoe selection! Antibiotic usage (Quinolone group) Cortisone Poor warm-up habits Achilles Tendonitis Symptoms: Pain behind ankle Pain just above the heel Increased pain during exercise Point tenderness over Achilles Tendon Worse in AM or after rest Scar like bump formation or thickening Achilles Tendonitis Management: PRICE Anti-inflammatory nutritional protocol + connective tissue support Ultrasound – 4-6X/week! Iontophoresis Myofascial Release (Foot, Calf Group) Manipulation/Mobilization of Foot/Ankle/Knee Dry Needle Therapy Orthotics Improve heel posting Heel Pad/Lift PRP?? Dorsi-Flexion Night Splint Avoidance and H2O running Traumeel topically 3X/day Swimmer’s Shoulder Causes: Faulty Stroke Mechanics Increased training intensity and/or volume Micro tears from overuse Excessive % of Freestyle swimming Weakness in Upper Traps and Serratus Ant. Weakness/Tightness in Posterior Rot. Cuff Hyper-mobile Shoulder Swimmer’s Shoulder Symptoms and Signs: Pain with Freestyle Forward Shoulder Slouch while sitting Winging of Scapula A.C. Jt. Tenderness Biceps Tendon, S.S. Tendon tenderness Reduced strength in S.S. and I.S. muscles Moderate shoulder Jt. laxity Swimmer’s Shoulder Management/Prevention: Establish bilateral breathing pattern Employ symmetrical body rotation Avoid Thumb First H2O entry Employ flat hand, finger tip first entry Open up chest muscles Think “shoulders back, chest forward” Avoid midline cross over at front of stroke *Employ High Elbow Catch and Pull Technique Strengthen External Rotators for Scapula Stability (Shoulder Horn!) Swimmer’s Shoulder Management/Treatment: PRICE Nutritional Anti-inflammatory protocol! Electrical Stimulation Trigger Point Therapy Iontophoresis Dry Needle Therapy Mobilization/Manipulation (Cervical, thoracic spine, shoulder, scapula, elbow, wrist/hand – upper kinetic chain) Myofascial release Tx. – shoulder girdle, pectorals Topical Traumeel Shoulder rehabilitation protocol for A.C. Jt. Decompression (see shoulder rehab protocol) ITB Syndrome **ITB Acts as a Stabilizer during running** Causes: Road Pitch Running Excessive Pronation/Supination Leg Length Discrepancy/Pelvic Un-leveling Varus knees (Bow legged pattern) Gluteal & Quad Tightness/Weakness Inadequate warm-up and/or cool down Excessive Hill running (up or down) Toed in position in cycling Excessive Breast stroking Excessive wear on outside heel edge of running shoes Weak Abductors (Glute Med.) ITB Syndrome ITB Syndrome Symptoms: Pain @ lateral aspect of knee Pain below knee (lateral aspect – attachment) Pain @ lateral lower thigh Pain @ lateral hip Pain increases with descending stairs and transitioning up from sitting Pain increases with heel strike ITB Syndrome Management/Treatment: PRICES Topical Traumeel + (DMSO) + Biofreeze Correct biomechanical distortion Orthotics cast to correct pedal imbalances Kinesiotape knee and/or hip Transverse Friction Massage Physiotherapy modalities (EMS, Ultrasound and Iontophoresis) Chopat type stabilizing brace Myofascial release @ Gluteal group, Quads, Lat. Hams, Gastrocnemius Restore strength to VMO to facilitate medial glide of patella Foam Roller! ITB Stretches Sciatica Discogenic: Bulging or herniated disc causing compression/irritation of sciatic nerve. Piriformis: Deep Gluteal muscle causing compression/irritation of sciatic nerve Sciatica Symptoms: Pain in gluteal and/or down back of thigh and leg into ankle/foot Burning/aching/tingling down thigh/leg/foot Weakness and/or numbness down extremity Constant pain in unilateral gluteal muscle Hip Pain Increased pain with straining, cough, sneeze Sciatica Symptoms (cont.): Diff. Diag. with Piriformis: Pain/dull ache in gluteal Pain after prolonged sitting Pain increases with stairs or inclines Sciatica Causes: Spinal Stenosis DDD DJD Spondylolisthesis Disc Herniation Trauma to back and/or hip/gluteal region Training with mechanical imbalances in kinetic chain Sciatica Treatment/Management: Diff. Diag. with exam and MRI Discogenic: PRICES Electrotherapy (EMS, Iontophoresis) Traction, Inversion Tx. Aggressive Nutritional Anti-inflammatory protocol!!! Correct Biomechanical imbalances Dry Needle Therapy and Acupuncture Training modification/low impact Resistant cases: Prescription NSAIDS, Prednisone, Muscle Relaxers Epidural Injections, Surgical Consult Sciatica Piriformis: Trigger point therapy Myofascial release tx. Correct biomechanical imbalances Electrotherapy (EMS, Ultrasound, Iontophoresis) Dry Needle Therapy Orthotics and/or running shoe modifications Foam Roller! Piriformis stretches Epsom Salt Bath Kinesiotape Sacroiliac Syndrome Large joint connecting the sacrum to the ilium bilaterally via ligaments and cartilage Symptoms: Pain over one SIJ Referred pain to the buttock, hip, groin and posterior thigh Tenderness over the SIJ Sacroiliac Syndrome Causes: DJD Changes Pregnancy – late effects Pelvic Un-leveling Pronation Poor shoe selection + extended wear Road Pitch Excessive tightness in LB and/or Hips Sacroiliac Syndrome Management: PRICES Diff. Diag. with exam (Gillet, provocation…) X-Ray Correct biomechanical imbalances Orthotics and/or modify shoe wear Gait Analysis Spine, Hip, Foot, SIJ Mob./Manipulation Foam Roller @ Gluteal group, lower back, hip flexors, hams and quadriceps Physiotherapy modalities (EMS, US, Iontophoresis) Topicals (Traumeel, DMSO, Biofreeze) Training modification Plantar Fasciitis Microtears and microruptures of the thick fibrous band of connective tissue originating @ bottom surface of calcaneous and extending along sole of foot toward toes Symptoms: Pain @ underside of heel Pain is most intense with first steps of day Painful dorsi-flexion Tight calf muscles Most likely 40-60yrs. Women>Men (Prevent!) Plantar Fasciitis Causes: Pronation and/or Supination Tight Soleus and Gastrocnemius Faulty Foot/Ankle biomechanics Prolonged shoe wear Road pitch Speed/Track training Excessive mileage or training intensity Improper training cycle pattern Age! Plantar Fasciitis Management: Diff. Diag.: MRI, Diagnostic Ultrasound and examination (dorsiflexion of foot, ankle and great toe while knee is extended) R/O Metatarsalgia, Heel Spur PRICE Orthotics cast Kinesiotape Myofascial release @ Calf group Stretching of both calf muscles and Achilles Rolling TX with cylindrical device, tennis ball Manipulation of foot/ankle/knee/hip/pelvis for ROM and alignment Ultrasound tx. Hot Water Immersion Radio Frequency Ablation (Extracorporeal shockwave therapy)?? PRP Medial Tibial Stress Syndrome “Shin Splints” Periosteal inflammation due to overuse and pulling of the muscle from its muscle/tendon origin Symptoms: Pain @ inside/back of Tibia Dull Ache progressing to sharp Pain starts with activity, reduces then increases again at or near end of activity Swollen lower leg Redness Lump and/or bump @ lower leg Pain with ankle/foot/toe plantar flexion Medial Tibial Stress Syndrome Causes: Increase in training intensity and/or mileage Running down-hill Uneven running surfaces and road pitch Weak dorsiflexors and/or stronger plantars Over-pronation Inadequate calcium intake Compensation Shoe fatigue Medial Tibial Stress Syndrome Management: PRICES Kinesiotaping and Compression Hose Orthotics cast Manipulation/Mobil. Of Foot, Ankle, Knee, Hip and SIJs Clear out imbalances @ External rotators of hip, Hip Flexors (Psoas), and Adductors Reduce volume and cross train Nutritional Anti-Inflammatory protocol Topicals: Traumeel + DMSO + Biofreeze Iontophoresis Meniscal Tears Meniscus: Rubbery C-Shaped disc of cartilage attaching to the tibia that act as shock absorbers Symptoms: Painful “Pop” Gradual stiffness ensues Gradual swelling ensues “Catching” or “Locking” “Giving Way” feeling occurs Loss of ROM Meniscal Tears Causes: Squatting Twisting Knee Degenerative changes Age Biomechanical Imbalances Repetitive Stress Meniscal Tears Management: PRICES R/O degree of tear (minor, moderate, severe) via MRI Kinesiotape Physiotherapy modalities (EMS, Iontophoresis) Biomechanical adjustments @ kinetic chain Orthotics Strengthen Quadriceps Training modification (pool) Nutritional anti-inflammatory protocol Nutritional connective tissue protocol HA, Orthovisc, Cortisone injections?? TIME Adrenal Fatigue Stress whether physical, emotional or chemical exhibits a response that stimulates the release of catecholamines (hormones) and taxes the endocrine system (H, P, T, A) The severity and longevity of the stress response as well as the adaptive capacity of the person will determine the resultant affects!! Adrenal Fatigue Symptoms: Fatigue! Blood Sugar Fluctuations >BP and >HR Depressed Immunity Increased fat storage Depression (decreases Serotonin) Elevated cortisol levels promote Inflammation Altered sleep quality despite exhaustion Tight muscles and aching joints Adrenal Fatigue Causes: STRESS!!! Lifestyle (exercise, nutrition, work and sleep habits) Environmental (exposure, chemicals, toxins) Worry, guilt, frustration, anxiety, depression GI disturbances, CVD, Chronic pain, etc. Adrenal Fatigue “The story is complicated, the intervention is simple.” Jeff Bland Diagnosis: Adrenal Fatigue Signs and Self Tests Health history, clinical evaluation, applied kinesiology assessment, dietary assessment Lab work – biomarkers for stress, fatigue, etc. (CBC w/Diff, CMP, ANA, CRP, HgbA1C, Vit D, Vit B12, Thyroid, EBV, Lyme, 24 hour urinary cortisol ASI and/or Neuro-Endocrine Comprehensive panel – salivary/urine - precise measuring of adrenal hormone status Adrenal Fatigue Management: Nutrition: Consume whole, fresh, organic foods Eat small frequent meals Identify and Address food allergies Sleep hygiene (Neuro-sleep panel for def.) Adaptogens!! (Tulsi, Rhodiola, Ginseng, Cordyceps, Shisandra, etc.) Glandular extract – adrenal Amino Acids - L-Tyrosine, L-Taurine, L-Theanine Inositol, GABA, DHEA, Pregnenolone Vitamins - > B5, B6, C Support as needed based on labs, upstream involvement! Degenerative Disc/ Joint Disease Gradual breakdown of joint substances such as cartilage, hyalgin, proteoglycans etc. The loss of these critical tissues deplete the joints and musculo-skeletal system with much needed support, cushion and lubrication!! DDD and DJD can lead to pain and significant mal-adapted compensatory patterns DDD and DJD generate inflammation DDD and DJD create loss of ROM and overactivate adjoining muscles DDD/DJD Causes: Age Repetitive Stress and Over-use Excessive loads/Resistance training Excessive body weight Biomechanical and Structural imbalances! Deficient nutrition (Omega 3s, Bioflavonoids, Silica, Manganese, Vitamin C, Amino Acids) Inactivity, prolonged postures (sitting/standing) Poor intersegmental joint function (Jt. Play) DDD/DJD Symptoms: Joint Pain – Sharp and/or Ache Referred Pain – Primary and Secondary HyperAlgesia Mechano-receptor pain Loss and Painful ROM Swelling and localized inflammation Crepitous Excessive Stiffness Frequently pain lessens with activity DDD/DJD Management: Diff. Diagnosis with X-Ray, CT and/or MRI Perform Wt. Bearing imaging to assess for biomechanical causes!! (MRI, X-Ray) Aggressive physiotherapy (EMS, US, Iontophoresis, ICE/MH) Aqua therapy – Exercise and Epsom Salts baths Anti-inflammatory nutritional protocol!!! Joint integrity nutritional protocol!!! Avoidance of pro-inflammatory mediators (Grains, Dairy) Joint mobilization/Manipulation at and adjacent joints (ROM and Align) CV exercise with Joint Friendly movements (Erg, Bike, Swim, etc.) Orthopedic Intervention - Surgery or Hyalgin/Orthovisc when applicable Spinal – Decompression Orthotics Brace and Compression Topicals!! Myofascial Release and Foam Roller to ease Joint compression Lowe Extremity Stress Fractures Partial Fracture in bone caused by repetitive loading. Usually an acute onset/mechanism of injury but may be unaware due to gradual nature. Can progress to acute fracture. Lower Extremity Stress Fracture Symptoms: Acute onset pain after long training session Pt. tenderness over FX site Pain dec. with rest and inc. with activity Aching and Throbbing late at night at rest Swelling, Heat and Radiating over FX site Lower Extremity Stress Fracture Causes and Characteristics: Non-Critical: Heal well and full return to sport after 6-8 weeks or relative rest Critical: Non-union of bone after 6-8 weeks Due to poor blood supply (Ant. Tibia and Distal Tibia (Malleolus) – slow healing Increase in training mileage/intensity Non-cycling of training surfaces Poor Shoe dynamics or over-wearing Poor Heel Posting No Metatarsal Support Pronation Biomechanical imbalances Gait imbalances Inadequate osseous nutrition Inadequate strength training Lower Extremity Stress Fracture Management: Diff. Diag.: X-Ray inadequate! MRI , Bone Scan!! PRICES 6-8 week “Relative Rest” in non-critical FX. (H20, Alt. CV work) Aggressive Bone Nutrition: Vitamin D3 (5K) IU, K2 (45mcg), MCHC (2Kmg), Ca (500), Mg (250mg), Choline Stabilized Orthosilicilic Acid (Silicon) (3mg), Horsetail (10ml) Increase Dark Green Veggies, Cruciferous!! EMS, Iontophoresis Orthotics Correct Biomechanical Distortion Patterns Kinesiotape!, Compression hose Brace/Cast/Boot and Ortho eval. in critical stress fxs. F/U with Gait Assessment Revisit appropriate shoe design Strength training Rotator Cuff Tendonopathy In response to physical training demands, the RC Tendons increase in diameter and thickness & consequently tensile strength Excessive training or poor technique leads to significant collagen synthesis (Type 3) rather than functional Type 2. Rotator Cuff Tendonopathy Symptoms/Mechanism: Elevated pain sensitivity due to increased development of nerve and blood vessels (neovascularization) This leads to degenerative changes Weaken Tendons Leads to Impingement Syndromes Adjacent Bursa inflames! Pain in front of shoulder (Aches!!) Pain radiates down arm but not below elbow Pain increases at night and if lying on affected side Painful arc movement – up or down Short Pectorals and anterior shoulders!! Intrinsic shoulder/RC muscle weakness Scapula rhythm altered! Inadequate extension emphasis Rotator Cuff Tendonopathy Management: Diff. Diag.: MRI, Clinical Examination PRICES Physiotherapy (EMS, US/Phonophoresis, Iontophoresis) Dry Needle Therapy Myofascial Release Tx. Manipulation/Mobilization @ Shoulder & spine Aggressive Nutritional Anti-inflammatory protocol Aggressive Connective Tissue Protocol Topicals! Kinetic Rehabilitation - RC isolation with progressive resistance (tubing), Pendulum, Shoulder retraction/extension based movements, scapula rhythm Open shoulder girdle and pectorals Evaluate swimming form, weight training techniques! Avoidance of overhead and push movements temporarily Orthopedic Eval. (Cortisone and/or decompression in difficult cases)