TB Pericarditis by Gay Gisselle Quimbao 6-17-2010
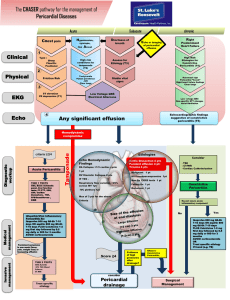
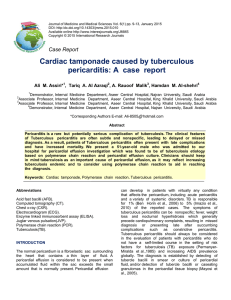
advertisement

"The heart has reasons that reason does not understand." Jacques Benigne Bossuel “Achy Breaky Heart” Quiambao, Gisselle T., M.D. June 17, 2010 Objectives To discuss the protean extrapulmonary manifestation of Tuberculosis To discuss the management and approach to a patient with pericardial effusion and Tuberculous Pericarditis General Profile E.M.P 30 year old Male Filipino Engineer History of Present Illness 7 months PTA intermittent cough (+) yellowish sputum (-) dyspnea (-) fever (-) night sweats (-) weight loss History of Present Illness Medical Consult done: Chest X-Ray: Normal Medication: Butamirate Citrate Outcome: temporary relief of cough but not resolved History of Present Illness 6 months PTA cough recurred (+) yellowish sputum (-) dyspnea (-) fever (-) night sweats (-) weight loss History of Present Illness Pulmonary consult: AFB smear x 3 days: negative He was treated as a case of Allergic cough Medication: Desloratadine Outcome: temporary relief of cough History of Present Illness 5 months PTA (+) cough recurred yellowish sputum (-) fever (-) night sweats Pulmonary follow up Spirometry : mild obstructive ventilatory defect Impression: Bronchial Asthma History of Present Illness 4 months PTA palpitations intermittent, sudden, occurs during exertion and even at rest (-) cough (-) dyspnea (-) syncope (-) chest pain (-) fever (-) heat or cold intolerance (-) tremors History of Present Illness Cardiology consult: 12L ECG : Sinus tachycardia, left atrial abnormality, non specific ST wave changes, Incomplete RBBB 2D Echo : Mitral valve prolapse. LV posterior wall hypertrophy 24 Hr Holter Monitoring: Rare episodes of PACs and PVCs History of Present Illness 2 months PTA (+) Shortness of breath Recurrence of cough yellowish sputum (+) 15 kg weight loss (-) fever Pulmonary follow up Impression: Allergic cough History of Present Illness 1 month PTA Impression: Pulmonary Consult Bronchial Asthma Medications: Acetylcysteine Loratadine + Bethametasone Levofloxacin Salbutamol + guiafenesin + bromhexedine History of Present Illness 2 weeks PTA cardiomegaly, Chest xray clear lungs Impression: Upper Respiratory Tract Infection Medication: Co-amoxiclav Salbutamol expectorant History of Present Illness 10 days PTA patient developed dyspnea (+) cough - yellowish sputum Echo : Pericardial effusion Admitted and treated as a case of CAP and Heart Failure 2D History of Present Illness Few hours PTA dyspnea persisted (+) cough - yellowish sputum ADMISSION Review of Systems: (+) 15kg weight loss (-) headache (-) dizziness (-) blurring of vision (-) colds (-) nape pains (-) vomiting (-) diarrhea (-) polyphagia (-) polydipsia (-) polyuria (-) dysuria (-) myalgia (-) athralgia (-) abdominal pain Past Medical History (+) Allergic cough (-) known PTB exposure Family History (+) Hypertension - Father (+) Diabetes Mellitus - Mother (-) Asthma (-) Pulmonary Tuberculosis Personal and Social History Non smoker Occasional alcoholic beverage drinker No recent travel / exposure to TB Physical Examination GS: conscious, coherent, ambulatory, oriented VS: BP 120/90 CR 73, RR 20 T 36.9C Wt. 115lbs HEENT: (+) subconjunctival hemorrhage on the left eye, tonsils not enlarged, no cervical lymphadenopathy, JVP 5 Lungs: symmetrical chest wall expansion, no lagging, no retractions, clear breath sounds bilateral. Physical Examination Heart: Quiet precordium. No heaves, thrills or lifts, regular rhythm, S1 and S2 were soft, muffled, with 2/5 friction rub heard at xiphoid process Abdomen: flabby, normoactive bowel sounds, soft, non tender Extremities: no edema, no cyanosis, no joint swelling, no active dermatoses. Salient Features Dyspnea Cough >1 month Weight loss Hoarseness of voice No fever Previous finding of pericardial effusion on 2dEcho (+) Friction Rub Clear lungs AFB smear (-) Chest X-ray cardiomegaly Admitting Impression: Pericardial Effusion etiology to be determined To consider Pulmonary Tuberculosis On Admission Chest X-Ray – normal, possible mild cardiomegaly 12 Lead ECG 2d Echo CBC 2dEcho Ejection fraction of 59%. Thickened mitral leaflet and pulmonic leaflets. Thickened cordae tendinae. Moderate to severe pericardial effusion. Color Flow Doppler study: Mitral, Tricuspid and Pulmonic regurgitation mild. Complete Blood Count 4/27/10 Hemoglobin Hematocrit 15.4 45.3 WBC Eosinophils Segmenters Lymphocytes 16.6 1.00 82.00 11.00 Monocytes Platelet 6.00 303,000 Infection Referral to Infectious Diseases Pericardial Effusion Referral to TCVS nd 2 Hospital Day Sputum AFB x 3 days Sputum culture ESR UTZ of the upper abdomen CT scan Symptom: Hoarseness of Voice t/c Pulmonary TB with TB Pericarditis t/c Laryngeal TB Medications: HRZE quadtab 5 tabs/day (Day 12) Prednisone 30 mg/tab, 1 tab 2x a day Ultrasound of the upper abdomen Minimal ascites Gallbladder polyp Normal Liver, spleen and kidneys Incidental finding of bilateral pleural effusion Sputum AFB – Negative for 3 days Sputum culture - ESR – 16 mm/hr CT scan – Pericardial effusion PLAN: Periardiostomy Flexible Nasopharyngolaryngoscopy Normal larynx 5 1 6 2 3 7 6 4 1=vocal cords, 2=vestibular fold, 3=epiglottis, 4=plica aryepiglottica, 5=arytenoid cartilage, 6=sinus piriformis, 7=base of the tongue Nasopharyngolaryngoscopy TB Laryngitis Tuberculosis of the upper aerodigestive tract is a rare entity. Incidence is less than 1% of all tuberculosis cases. Pathogenesis is either primary or secondary. Primary: direct inoculation Secondary: haematogenous or lymphatic spread TB Laryngitis Clinical presentation: Dysphagia Hoarseness Chronic cough. Posterior half of the larynx. TB Laryngitis Localization in the anterior half of the larynx now occurs twice as often Vocal cords (50-70%), False cords (40-50%) Epiglottis, aryepiglottic folds, arytenoids, posterior commisure and/or subglottis (1015°%). Laryngoscopic features mimic malignancy in many cases. LARYNGEAL TUBERCULOSIS CLINICALLY SIMILAR TO LARYNGEAL CANCER S. K.Verma1, Sanjay Kumar Lung India 2007; 24 : 87-89 TB Laryngitis About 6% have no evidence of pulmonary disease 30% show positive early morning urine culture Biopsy of the primary growth itself is diagnostic and may show caseating granulomatous inflammation. Microbiological confirmation, though desirable, may not always be possible. LARYNGEAL TUBERCULOSIS CLINICALLY SIMILAR TO LARYNGEAL CANCER S. K.Verma1, Sanjay Kumar Lung India 2007; 24 : 87-89 Management The response to Anti-TB treatment is good. LARYNGEAL TUBERCULOSIS CLINICALLY SIMILAR TO LARYNGEAL CANCER S. K.Verma1, Sanjay Kumar Lung India 2007; 24 : 87-89 Back to our patient… Nasopharyngolaryngoscopy Hoarseness secondary to Laryngeal TB (Evidence of Reflux Disease Noted) Nodular swelling of the right vocal fold Treatment: Continue HREZ treatment Fexofenadine 120mg/tab 1 tab daily at bedtime Back to our patient… 2d Echo: Pericardial effusion CT scan of the chest Minimal pericardial effusion Plan: Pericadiostomy Potential algorithm for managing patients with a moderate to large pericardial effusion Little, W. C. et al. Circulation 2006;113:1622-1632 Copyright ©2006 American Heart Association Back to our patient… Pericardiostomy Problem: with biopsy Pericardiostomy not completed due to thick and gritty pericardium. Pericardial biopsy Pericardial Effusion Histopath: Caseating granulomas consistent with tuberculosis, pericardium Plan: Pericardiectomy Normal Pericardium Normal Myocardium Pericardium 10x the normal thickness OR Findings Multiple Casseating granulomas adhering to the pericardium and myocardium. Multiple hilar formations on the surface of the heart Histopath: Anterior pericardium 5/8/10: Caseating granulomas consistent with tuberculosis, pericardium Summary 30 y/o male Chronic cough Dyspnea Chest X-Ray – clear lungs, cardiomegaly 2dEcho – Pericardial Effusion Sputum AFB Negative + Laryngeal TB + Tuberculosis – pericardium + Histopath findings of Tuberculosis Final Diagnosis: Disseminated Tuberculosis TB Pericarditis with Pleural effusion Laryngeal Tuberculosis Anterior Pericardiectomy Extrapulmonary Tuberculosis Extrapulmonary tuberculosis occurs in any age group More in the 2nd and 3rd decades of life Male preponderance. Fever, anorexia, abdominal pain and cough are more common in those with positive chest xrays. Extrapulmonary Tuberculosis* Emelita P. Ang, M.D.,Estelita M. Quimosing, M.D. and Bienvenido D. Alora, M.D [Phil J Microbiol Infect Dis 1982; 11(2):115-123] Extrapulmonary Tuberculosis Proportion in all TB in USA : 7% (1963) to 18% (1987) to 20% (now) Increase maybe due to HIV infection More in minorities and foreign-borns Lymphatic TB (30%) > Pleural TB (24%) > Bone and joint TB (10%) > Genitourinary TB (9%) > Miliary TB (8%) > Meningeal TB (6%) (New York, 1995) Extrapulmonary Tuberculosis A negative chest x-ray does not exclude the presence of extrapulmonary tuberculosis because it can present as pleural effusion, mediastinal mass, metastatic cancer, pneumonia, pneumothorax, pulmonary neoplasm and atelectasis. Extrapulmonary Tuberculosis* Emelita P. Ang, M.D.,Estelita M. Quimosing, M.D. and Bienvenido D. Alora, M.D [Phil J Microbiol Infect Dis 1982; 11(2):115-123] Pericardial Effusion Patients presenting with a pericardial effusion for the first time are usually hospitalized to determine the cause of the effusion and to observe for the development of cardiac tamponade. Disease-specific and adjunctive therapy is given to those in whom pericarditis represents one manifestation of systemic illness. Management of Effusive and Constrictive Pericardial Heart Disease Circulation Journal of American Heart Association 2002;105;2939-2942 Brian D. Hoit Pericardial Effusion In the absence of tamponade or suspected purulent pericarditis, there are few indications for pericardial drainage Large effusions (when associated with pericarditis) that are unresponsive to nonsteroidal anti inflammatory drugs, corticosteroids, or colchicine, and unexplained effusions, especially when tuberculosis is suspect or when present for 3 months, warrant pericardiocentesis Management of Effusive and Constrictive Pericardial Heart Disease Circulation Journal of American Heart Association 2002;105;2939-2942 Brian D. Hoit Tuberculous Pericarditis Tuberculous pericarditis develops secondary to contiguous spread from mediastinal nodes, lungs, spine, or sternum, or during miliary dissemination. The onset may be abrupt or insidious with symptoms such as chest pain, dyspnea, and ankle edema. First stage: diffuse fibrin deposition Second stage: serosanguinous pericardial effusion then develops. Lymphocytes, monocytes and plasma cells replace the PMNs Third stage: effusion absorbed and the pericardial thickens Fourth stage: pericardial space is obliterated by dense adhesions and many granulomas are replaced by fibrous tissues Tuberculous Pericarditis Cardiomegaly, tachycardia, fever, pericardial rub, pulsus paradoxus, or distended neck veins may be found on examination. Pericardial biopsy yields a definitive diagnosis more often than pericardial fluid alone. Why was it missed? The diagnosis of TB based solely on smear microscopy—a method dating from the late nineteenth century—is not sensitive. Many patients with pulmonary TB and all patients with exclusively extrapulmonary TB are missed by smear microscopy. Harrison’s Principles of Internal Medicine 7th ed Accuracy of Sputum AFB Smear It is the simplest, most rapid procedure to detect the presence of acid-fast bacilli. It will take 5,000 to 10,000 bacilli per ml of sputum to detect their presence in smears. Sensitivity is 22 to 43% in single smear, but detection is improved by examining multiple specimens. Accuracy of AFB Smear Techniques at the Health Center LevelConcepcion F. Ang, RMT, Myrna T. Mendoza, M.D. and Tessa Tan Torres, M.D.**(Phil J Microbiol Infect Dis 1997; 26(4):153-155) Bacterial pericarditis is treated with appropriate systemic antibiotics, surgical exploration, and drainage. Pericardial effusion occasionally responds to the addition of corticosteroids Management of Effusive and Constrictive Pericardial Heart Disease Circulation Journal of American Heart Association 2002;105;2939-2942 Brian D. Hoit Management of Extrapulmonary TB Treatment of pulmonary tuberculosis = extrapulmonary tuberculosis. Extrapulmonary: 6-month course of therapy The addition of corticosteroids is recommended for patients with tuberculous pericarditis and tuberculous meningitis. American Thoracic Society, CDC, and Infectious Diseases Society of America MMWR: June 20, 2003 / Vol. 52 (RR11): 1-77 Management of Extrapulmonary TB The risk of progression to constrictive pericarditis or mortality is not altered by corticosteroids. Open pericardial drainage is favored over repeated pericardiocentesis. Conclusion Extrapulmonary involvement can occur in isolation or along with a pulmonary focus Extrapulmonary sites of infection commonly include lymph nodes, pleura, osteoarticular areas, cardiovascular, larynx Conclusion Not all patients with Extrapulmonary TB will present with Pulmonary TB Patients presenting with a pericardial effusion for the first time are usually hospitalized to determine the cause of the effusion and to observe for the development of cardiac tamponade. Conclusion Adjunctive corticosteroids may be beneficial in patients with, tuberculous pericarditis, or miliary tuberculosis along with standard Anti-Tuberculosis agents Thank you