Adrian`s Powerpoint presentation here
advertisement
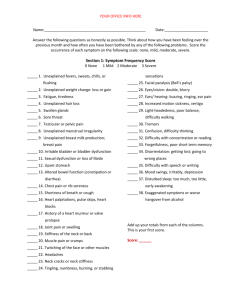
Medically Unexplained Symptoms Adrian Flynn Consultant Liaison Psychiatrist January 2013 Aims Be contentious Explore current practice Consider costs and prevalence Empathy Psychological Explanation New classifications / way of thinking General tips Format 45 mins presentation and discussion 15mins trainee’s experience BREAK 30 mins Group discussion and feedback 20mins Consultation / suggestions 10mins Discussion / re-cap MUS Medically Unexplained Symptoms (MUS) are persistent bodily complaints for which adequate examination does not reveal sufficient explanatory structural or specified pathology. Never Have Your Dog Stuffed 3 Recent Referrals Miss P Ms F Mrs T Is this familiar? What do you want to say to these patients? What would you have said to them 20years ago? Do you use diagnostic terms with these patients? How were you taught or where did you learn about the management of these patients? What guidelines do you follow? Do doctors manage this consistently? How do you feel about these patients? Classification Somatisation Disorder Somatoform pain disorder Hypochondriasis Functional Somatic Syndromes Dissociative Disorder Conversion disorder Are you comfortable with any of these? Are your patients? But does it really matter? 22% of all people attending primary care have subthreshold levels of somatisation disorders A further 5% of individuals have clinical somatisation disorders They account for 8% of all prescriptions 25% outpatient care 8% inpatient bed days and 5% accident and attendances 50% more likely to attend primary care 33% more likely to attend acute secondary care 20% of MUS patients account for 62% of spend Signs, symptom ill-defined conditions ICD 6.3% in US healthcare 25% of new symptoms in primary care – but one visit only But 10% (2.5% of total) are persistent More common in secondary care – 40% persist But does it really matter? Clinic Prevalence (95% CI) Chest Cardiology Gastroenterology Rheumatology Neurology Dental Gynaecology Total 59% 56% 60% 58% 55% 49% 57% (46-72) (46-67) (45-73) (47-69) (45-65) (37-61) (50-68) 56% (52-60) Nimnuan et al 2001 J Psychosom Res But does it really matter? The NHS cost in England amounts to £3.1Bn (2008/9) with a further £5.2Bn attributable to lost productivity and £9.3Bn reduced quality of life Total £14Bn Sainsbury Centre for Mental Health - £2.8Bn Equates to £25M – £130M per year in Cornwall Diabetes? Bermingham S, Cohen A, Hague J, Parsonage M. The cost of somatisation among the working-age population in England for the year 2008/09 Mental Health in Family Medicine No health without mental health: A cross Government mental health outcomes strategy for people of all ages Supporting document – The economic case for improving efficiency and quality in mental health.2010 Department of Health Scottish Neurological Symptoms Study N = 3782 - ‘To what extent can the patients symptoms be explained by organic disease?’ Not at all Somewhat Largely Completely - 12% 19% - 24% 45% 12 Month Outcome of the 31% with MUS 60% 50% 40% 30% 3 months 12months 20% 10% 0% Much better Just the same Much Worse Do Medically Unexplained Symptoms Matter? Carson et al. J Neurol Neurosurg Psychiatry 2000;68:207–210 N = 300 Similarly categorised Similar levels of physical disability Higher total symptom count and pain in those with lower organicity Higher levels of anxiety and depression in the lower organicity group 70% vs 32% Change of Diagnosis Completely Largely Somewhat Not at all - 0.3% 2% 0.5% 2% At follow-up only 4 out of 1030 patients (0.4%) had acquired an organic disease diagnosis that was unexpected at initial assessment and plausibly the cause of the patients’ original symptoms. Underlying Pathology Slater 1965 Repeats Roth, Trimble/Mace, Crimlisk – 2-4% Kooiman et al - 5 out of 284 Stone et al – 4 out of 1030 ?Negligent to continue to investigate Medical Generalism RCGP 2012 Real conversations are required Real conversations require real empathy Empathy requires understanding Understanding needs to be conveyed Understanding combines - biomedical knowledge - biographical knowledge Conveying requires communication skills Is there a way of doing things differently? Never Have Your Dog Stuffed The Development of Symptoms What is really going on? We tend to respond to people in the way we anticipate they will treat us and From how others relate to us, we learn how to relate to ourselves. Personal biographical history Reciprocal roles Abuse and Neglect What is really going on? Mother Caring Valuing Child Cared for Valued Child/Self Caring Valuing Child/Self Cared for Valued What is really going on? Abuse and Neglect Withholding (limited) Contemptuous (disgusted) Deprived (unsatisfied) Contemptible (disgusting) Demanding Unreasonable Overwhelmed Inadequate Critical Rejecting anger Crushed Rejected Hopeless Powerful Imposing Bullying Disempowered Silenced Bullied What is really going on? We tend to respond to people in the way we anticipate they will treat us A person enacting one pole of a RR procedure may either: 1. Convey the feelings associated with the role to others, in whom corresponding empathic feelings may be elicited (identifying) or 2. Seek to elicit the reciprocating response in the other’ (reciprocating) But does it really matter? Could we make the argument that modern medicine is spending 30-50% of its time, poorly managing the consequences of abuse and neglect? ‘A ghost in the machine?’ Descartes – ‘substance’ ‘lead the mind away form the senses’ Demertzi et al 2009 Disorders of Consciousness. N=2100, 53% mind and brain are separate 37% mind is fundamentally physical ‘A ghost in the machine?’ There is a doctrine about the nature and place of the mind which is prevalent among theorists, to which most philosophers, psychologists and religious teachers subscribe with minor reservations. Although they admit certain theoretical difficulties in it, they tend to assume that these can be overcome without serious modifications being made to the architecture of the theory.... [the doctrine states that] with the doubtful exceptions of the mentally-incompetent and infants-in-arms, every human being has both a body and a mind. ... The body and the mind are ordinarily harnessed together, but after the death of the body the mind may continue to exist and function. New Classifications Higher order constructs Less context dependant Less vulnerable to change Current FSS etc… Absence of biological correlates / points of rarity MUS Hypochondriasis Medical Illness Depression and Anxiety Somatoform Disorders Functional Somatic Syndromes text New Classifications Complex Somatic Symptom Disorder - health related anxiety - disproportionate concerns - excessive time and energy Bodily Distress Syndrome - cardiopulmonary - musculoskeletal - gastrointestinal - general What to do? Metabolic syndrome – knowing what to expect and what to do about it? Can we make it that straightforward? Expect and Enquire CFS + IBS + FMA NEAD / dissociation Functional neurology Pelvic / Abdominal / Vertebral Pain Dysuria / retention symptoms Dysmenorrhoea Anxiety / depression Start explaining and making the links Avoid ‘cure’ discussions / treatments Numbers needed to offend Medically unexplained Depression related All in the mind Stress related Hysterical Functional Psychosomatic Numbers needed to offend DIAGNOSIS All in the mind Hysterical Psychosomatic Medically unexplained Depression related Stress related Functional NNO 2 2 3 3 4 6 9 Don’ts Tell them that there is nothing wrong. Normalise. They are not normal for the patient. Say it is all in your mind Only reassure repeatedly Tell them there is nothing you can do to help. Give results of normal tests and reassure and think that this alone will help. Remove gall bladder, appendix, uterus, bowel, teeth Prescribe dependence forming drugs Retire them on grounds of ill-health Do’s Indicate that you believe the patient Explain how symptoms occur Explain what they don’t have Explain what they do have Emphasise that it is common Emphasise that it is reversible Emphasise that self-help is a key part of making a recovery Involve a carer and repeat the explanations Be honest and use praise Also Metaphors may be useful Brain playing tricks Use written information Get the family on side Consider Anxiety / Depression Use anti-depressant medication CBT – often re-framed Communicate and deal with the system Care Plan Improving well-being - relaxation / mindfullness - 5 a day - routine / pacing / structure / diary Managing a crisis - self-management / local support - clear plans for primary and secondary care Avoiding harm - in-built review - being clear that medicine can be harmful - dealing with the system - sharing information - dependence forming drugs Resources Diaries Self-management toolkit Boom and bust graph Mental Health 5 a day Relaxation – CD www.mentalhealth.org.uk www.neurosymptoms.org www.nonepilepticattacks.info www.NEADtrust.co.uk www.paintoolkit.org London Pilot 227 patients from 3 practices (0.84%) >£1M expenditure in 2 years £307k in GP time alone 1/5 had in-patient treatment - £250k Intervention (over one month) Reduced GP contacts by 1/3 (258 vs 375) Reduced investigations by 1/4 (54 vs 74) Training GPs Knowledge Practice Treatment Services / commissioning Aims Be contentious Explore current practice Consider costs and prevalence Empathy Psychological Explanation New classifications / way of thinking General tips A Service Clear point of entry One-stop-shop + Out-patients Liaison Psychiatry formulation CBT / GET Hypnotherapy (IBS) Mindfulness Physiotherapy / OT Pain / self management groups Managing the system Identify >/= 10 attendances in 2 years >/= 2 negative investigations in 2 years the symptom does not fit with known disease models or physiological mechanisms the patient is unable to give a clear and precise description of the symptoms symptoms seem excessive in comparison to the pathology Identify symptoms occur in the context of a stressful lifestyle or stressful life events patient attends frequently for many different symptoms the patient seems overly anxious about the meaning of the symptoms and has strongly held beliefs about a disease process causing the symptoms patient complains of pain in multiple different sites The End - Culture Change? Is this how we will be practicing medicine with these patients in 10 years time?