VITAL SIGNS presentationML 1
advertisement

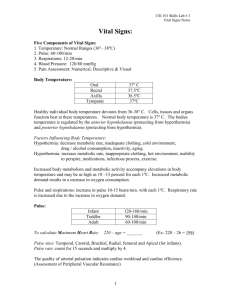
VITAL SIGNS Vitals Signs • 4 types(TPR & BP) – Temperature – Pulse – Respirations – Blood Pressure • Degree of Pain is frequently regarded as the 5th VS(pain scale 0-5) • Color of the skin, size of the pupils in the eyes and their reaction to light, level of consciousness, and patient’s response to stimuli • VS provide information about the basic body conditions of the patient **Earliest indicators of change in the body Temperature • Balance between heat production and heat loss in the body • Disturbances such as hypothermia (low temp) or pyrexia (fever) affects the body’s fluid balance • Factors affecting Temperature: Time of day(usually lower in morning), age, environmental temperature, exercise, menstrual cycle Body heat is created by - exercise food ingestion muscle tension hormones external factors such as clothing, blankets, etc. illness and infection excitement Heat loss occurs by - sweating/dilation of blood vessels respirations excretion(urine and feces) ***Starvation/fasting, sleep, decrease muscle activity, mouth breathing, & cold temperatures cause decrease in body temp Types of thermometers • Glass • Electronic • Topical/temp strip Temporal artery Normal Temperature Ranges – Axillary (under the armpit) **less accurate Taken for 5-10 minutes with glass or electronic thermometer 96.6F - 98.6F (1 degree less than oral) Oral Taken for 3 - 5 minutes with glass, paper, or electronic thermometer 97.6F - 99.6F (fever is anything over 100.6F oral) Rectal “core” **most accurate Taken 3-5 min with electronic or glass thermometer after inserting the thermometer 1 1/2 - 3 inches in the rectum 98.6 F- 100.6F (1 degree higher than oral) Tympanic(the ear) “core” Taken 1-2 sec with electronic thermometer 96.4F to 100.4F CLASSIFICATIONS OF FEVERS Slight= Moderate= Severe= Dangerous= Fatal= 99.6-101.0 F 101.0-102.0 F 102.0-104.0 F 104.0-105.0 F Over 106.0 F 37.5-38.3 C 38.3-38.8 C 38.8-40.0 C 40.0-40.5 C 41.1 C Hypothermia Low body temp below 95F rectally Can be caused by prolonged exposure to cold Death usually occurs if temp drops below 93F rectally Fevers/ Febrile (Pyrexia) Usually 100.4-101 orally is considered a fever Usually caused by infection or injury Afebrile means no fever is present or the temperature is within the normal range. Symptoms of Infection: elevated temperature chilling sensation malaise - feel ‘blah’ no appetite Hyperthermia Body temp exceeds 104F rectally Caused by prolonged exposure to hot temp, brain damage, or serious infections Immediate action to lower temp Temp above 106F can quickly lead to convulsions, brain damage, and death. Treatment for fever: • Tepid baths • Reduce room temp and amount of bedding • Force fluids • High calorie diet • Medications if necessary • **Fluctuations of 2-3 degrees increases metabolic rate and pulse rate (10 beats/degree) Before taking an oral temperature: Ask the patient - “Have you had anything to eat, drink or smoke in the last 15 minutes?” (If they have, wait 15 minutes to take the temp) Oral temps are not taken on – patients under the age of 4 or 5 patients who mouth breathe or have nasal congestion patients with a nasogastric tube patients on Oxygen patients who have had face/neck/nose/mouth injuries or surgery patients who are confused, restless, delirious, or unconscious patients who are paralyzed on one side of the body patients who has sore mouth Report all temperatures over 100.6F or 37.9C Immediately!! Rectal temps are used for infants and children under 3 yrs old and when the oral site cannot be used. Rectal temps are not taken on – patients who have had any rectal surgery/injury patient with inflamed hemorrhoids patients with bleeding from the rectum patients who have diarrhea patients who have heart disease patients who are confused or agitated Tympanic Membrane (ear) are not taken onpatients who have an ear disorder patients who have ear drainage Which method would you choose? -infants and children under the age of six -patients with respiratory complications that result in mouth breathing or use of supplemental oxygen -confused, disoriented, or emotionally unstable patients -patients with nasal obstruction Calculations PULSE POINTS Antecubital How to evaluate a pulse • • • • • Find pulse point Feel with pads of first two fingers No thumb Make sure you feel it well Time (count) for 30 seconds and multiply by 2 • If irregular you MUST count for a full minute CHARACTERISTICS OF PULSE RATE Beats/minute RHYTHM Regular or irregular VOLUME Strong, weak, thready, or bounding EXAMPLE RECORDING PULSE: Date, Time, P 82 strong and regular, Your signature & title Pulse - heart rate/minute (beat of the heart that is felt through the walls of arteries) **Most often taken at the radial artery *usually taken for 30 seconds and multiplied by 2, unless the heart rate is irregular **if the heart rate is irregular, the pulse must be taken Apically (at the apex of the heart in the chest) with a stethoscope for 1 Full minute Normal Adult pulse: Children: Infants: 60 - 100 beats per minute 70-110 beats/min. 100-160 beats/min -Slow pulse rate less than 60/ minute = Bradycardia, and must immediately be reported -Rapid heart rate over 100/ minute = Tachycardia, and must be reported **You must note the Rate, Strength of the pulse(volume) and Rhythm and document this Apical Pulse • Most accurate • Use for irregularity • Use in infants & children (difficult to count rapid radial pulse) • Auscultated(listen) NOT palpated(felt) – full minute • Stethoscope required • Apex – left, 5th intercostal space of ribs at middle of left clavicle. (2 to 3 inches to the left of the breastbone below the left nipple) EXAMPLE RECORDING: Date, Time, AP 84 strong and regular, Your signature & title. Heart Sounds Lubb – S1 – Apex – valves between chambers closing (bicuspid and tricuspid) Dupp – S2 – 2nd intercostal space at the sternal borders – pulmonary and aortic semilunar valves closing Abnormal Sounds • • • • S3 S4 Murmurs Rubs What may cause an increase in pulse? • • • • • • • Exercise Emotion (excitement, nervous, tension, stress) Disease(infection, cardio-vascular disease) Medications Fever Shock Age: younger=faster How about a decrease in pulse? • • • • • • • • Medications Depression Sleep Physical fitness Heart disease Coma Larger size Age Pulse Defecit • • • • Apical – radial = pulse deficit Requires 2 medical professionals Measure for full minute Discrepancy means trouble (weak heart, tachycardia) Respirations - number of breaths per minute -represented by 1 Inspiration (breathe in) + 1 Expiration (breathe out) Normal range for Adult Respirations: 12 - 20 breaths / minute Children: 16-25 breaths/min. Infants 30-50 breaths/min **You must document the symmetry of the chest on inspiration, depth, rhythm and any abnormal sounds heard Use words such as deep, shallow, labored, moist, difficult, & stertorous (abnormal sounds like snoring) Slow respirations less than 12/min = Bradypnea Rapid respirations over 20/min = Tachypnea Abnormal sounds: 1. rales - moist crackling sounds(fluid in air passages) 2. rhonchi - noisy breathing 3. stridor - ‘crowing’ on inspiration (usually will see the chest caving in with inspiration) 4. wheezing - whistling noises with inspiration or expiration(narrow bronchioles (asthma) Types of Breathing: Eupnea - normal breathing Dyspnea – difficulty/ labored breathing Orthopnea - difficulty breathing while lying down Apnea - no breathing Sterterous - noisy breathing that sounds like snoring Cheyne Stokes breathing - periods of deep labored breaths(dyspnea), followed by very short or no breaths(apnea), and repeat in cycles (occurs shortly before death) Kussmaul breathing: heavy labored breathing with a fruity odor Cyanotic- dusky, bluish discoloration of the skin, lips, nail beds. Counting Respirations 1. Stay in the pulse measuring position. 2. Watch the chest rise and fall. Determine the quality… 1. 2. 3. Depth (deep or shallow) Rhythm (regular or irregular) Count respirations by 30 seconds and multiply by 2 Let the patient think you are still taking pulse while counting! (Patients may breathe faster or slower when they are aware of this procedure) EXAMPLE RECORDING: Date, Time, R 18 deep and regular, Your signature and title Blood Pressure Evaluates… • The condition of the heart • The amount of blood forced from the heart and contraction • The condition of the arteries • The volume and viscosity (thickness) of the blood Blood Pressure pressure exerted on the walls of arteries when the blood is pumped out of the heart (Systolic BP), and the pressure left when the heart is at rest (Diastolic BP). Factors affecting Blood Pressure: Age pain disease salt consumption alcohol and drugs exercise emotions Equipment • • • • Sphygmomanometer Stethoscope Pen Paper Measured in millimeters(mm) of mercury(Hg) BP is normally measured in the brachial artery on the antecubital area (fold of arm opposite elbow). Systolic Diastolic • Systolic pressure- top number – The contraction phase of the heart. – The period of highest pressure. • Diastolic pressure –bottom number – The relaxation phase of the heart. – The period of lowest pressure. What Should Normal BP Be? • Normal BP is: – Systolic pressure less than 140 – Diastolic pressure less than 90 – Ideally both are less than 120/80 • Pre-hypertension >120 / >80 • Hypertension BP is when the systolic pressure is over 140 and/or diastolic is over 90. There are mild, moderate, and severe cases. Hypertension **Can cause a stroke (Cerebral vascular accident / CVA) **High blood pressure also damages the kidneys, heart and retina of the eyes Hypotension - a sustained systolic BP less than 90mm or diastolic BP less than 60mm **only dangerous with symptoms of shock: rapid weak pulse cold, clammy, pale/blue skin anxious dizziness Factors that affect blood pressure • • • • • • • Diseases Emotional status Techniques and equipment Position Activity level Medication Diet (caffeine, sodium) Pulse Pressure • Difference between systolic and diastolic (subtraction) • Systolic – Diastolic = Pulse Pressure • Normal 30-50 mmHg Sounds of blood pressure - Korotkoff Sounds tapping swishing knocking muffled silence Steps to Finding Blood Pressure B/P PREP Expose upper arm- palm up. Identify brachial artery. Place middle of cuff bladder over the brachial artery. Wrap cuff smoothly & snugly. Palpate the brachial or radial artery & inflate cuff. Note on the dial where you no longer feel pulse. Add 30 to this number to determine how high to pump up the cuff. OBTAINING THE BLOOD PRESSURE 1.Patient should be resting for 5 minutes prior to taking the reading 2.You must document the position the patient was in (sitting/lying) *Do not take the BP standing unless ordered that way 3. Use the correct size cuff 4. Use the brachial artery 5. Palpate the brachial artery and inflate the cuff 30mm above where the pulse disappeared. Deflate the cuff slowly(2-4mm/sec). Where you feel the pulse return, will be approximately what the systolic BP will be. 6.Note the number on the dial you first hear a beat(systolic number). 7. Keep listening and note the last number you hear a sound or until the sound disappears (diastolic number). 8. Deflate completely before re-inflating the cuff. Wait 30 seconds if you must recheck. 9. Once the cuff is inflated, immediately start slowly deflating or venous congestion will occur and the reading will be inaccurate Recording • BP systolic/diastolic • Example: BP 120/80 L arm sitting