Manual
dipstick
urinalysis
Lynne Powell
RN MSc IP PgCEd
INTRODUCTION
URINALYSIS is a simple non-invasive
diagnostic test which can provide a
glimpse into a person’s health
Objectives
Give an overview of the anatomy and
physiology of the urinary system
Explain how urine is produced and its
components
Describe the types of urine samples and
tests
Describe the requirements and procedure
for dipstick urinalysis using the manual
method
The urinary system
Organs of the urinary
system
Kidneys
Ureters
Urinary bladder
Urethra
The function of the urinary
system
The kidneys regulate: acid-base balance;
electrolyte concentration; extracellular fluid
volume (homeostasis).
The kidneys remove waste & water from the
blood stream and reabsorb vital nutrients.
The kidneys regulate the blood pressure.
The urinary bladder stores urine.
KIDNEY nephron
Formation of urine
HCO 3 – bicarbonate
NaCl – sodium chloride
K – potassium
H2O – water
H – hydrogen
NH3 - amonia
Components of urine
Components of urine
Collection requirements
Containers – white/red/green topped
Discuss.
Mid stream
Early morning
Sample storage < 2hrs or kept at 4c out of
direct sunlight - DISCUSS
Types of sample
Random – most common for infection.
Early morning urine (EMU) – has greater
Clean catch midstream (MSU) – genitalia
Timed – specific time of day, always discard the
24 hour – used for quantitative and qualitative
concentration of substances (micro-albumInuria).
should be cleaned, urine is tested for microorganisms for presence of infection (culture &
sensitivity).
1st specimen before testing.
analysis of substances.
Types of testing
Physical
Chemical
Microscopic
Physical examination of urine
Done with the naked eye, a very important
part of the test. Findings should be
documented.
Colour (affected by drugs, food, general
condition).
Turbidity (clear; cloudy, particles).
Volume.
Odour (affected by infection, diet)
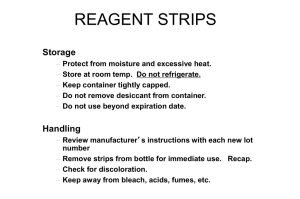
Chemical testing of urine
Usually done with reagent strips.
Used to determine body processes such as
carbohydrate metabolism, liver or kidney
function.
Used to determine infection.
Can be used to determine presence of drug or
toxic environmental substances.
Some chemicals that can be found in
urine (not normal components)
Ketones .
pH – acid/alkaline balance.
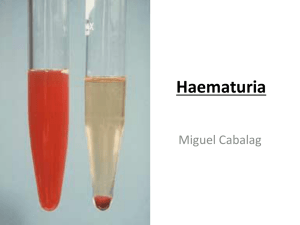
Blood
Bilirubin (urobilinogen)
Glucose
Protein
Nitrates
Leukocytes
drugs
Phenylketones – indicates PKU – a rare genetic disorder of one of the liver
enzymes. If left, can cause a build up of the chemical in the blood and brain
which can cause mental development issues and epilepsy – screened for in
babies 1st week of life with heel prick test.
Microscopic examination of
urine
Used to examine the elements not
visible without a microscope.
Centrifuge spins the urine to
separate substances.
• Cells
• Crystal
• Casts
• Bacteria
• Yeasts
• Parasites
Other tests
Pregnancy tests – EIA (enzyme
immunoassay test) used to detect human
chorionic gonadotrophin (hCG), secreted
by the placenta.
STIs - chlamydia
The manual
dipstick test
Do’s and don’ts
DO
Follow manufacturers instruction.
Ensure the sample is in the correct container for the
test required (red/white top).
Ensure correct reagent strips are selected for the
required test. Discuss.
Always check and record the appearance of the
urine sample.
Return the top on the reagent strip bottle.
TIMING IS ESSENTIAL for reliable results.
Do’s and don’ts
DON’T
Remove the desiccant from the reagant strip
bottle.
Touch the test areas of the strip.
Take out more strips than are required for
immediate use.
Quality control
Sample requirements
Patients should instructed on how to collect
the sample.
Sterile containers should be used to collect
the sample
All samples must be properly labelled with the
patient ID.
Ensure the sample is in the correct container
for the test required.
The first sample on waking should be used for
microalbumInuria as other samples may be
less concentrated.
Patient instruction
‘How should I collect and store a urine sample?” NHS choices (11/10/2013)
To collect a clean urine sample:
label
the container with your name, date of birth and the
date
wash your hands
men should wash their penis
women should wash their genitals, including between the
labia (lips around the entrance to the vagina)
start to urinate but don’t collect the first part of urine that
comes out
collect a sample of urine ‘mid-stream’ (see below) in a sterile
screw-top container
screw the lid of the container shut
wash your hands thoroughly
http://www.nhs.uk/chq/pages/how-should-i-collect-and-store-a-urinesample.aspx?CategoryID=69&SubCategoryID=692
Materials/equipment required
for dipstick testing
Reagent/test strips – in-date and stored
correctly
Watch
Urine sample in suitable container
Gloves
Good lighting
Access to hand washing and drying
Suitable room (sluice) for testing
Suitable waste disposal - discuss
Manual Test procedure
①
②
③
④
⑤
Wear gloves.
Ensure the sample is in the correct
container.
Check the appearance of the sample
and record results.
Ensure the strips have been stored
properly & are in-date.
Remove the cap, take out strip and
replace the cap on the bottle.
Manual Test procedure
⑥
⑦
⑧
Using the appropriate reagent strip
completely immerse all reagent areas
into the sample. Dip briefly and remove
immediately to avoid dissolving out the
reagents.
While removing the strip, run the edge
against the rim of the urine container to
remove excess urine.
Hold the strip in a horizontal position to
prevent possible mixing of chemicals
from the adjacent areas.
Manual Test procedure
⑨
⑩
After the appropriate time, compare test
areas closely with the corresponding
colour chart on the bottle label at the
specified time. Hold the strip close to the
colour blocks and match carefully.
Always record results.
Sources of error
Incorrect dipping of reagent strip.
Incomplete wetting of strip.
Incorrect storage of strips – always check
manufacturers instructions.
Sample error – sample must be allowed to return to
room temperature, non sterile containers; sample
needs to be fresh for best results.
Contamination of the reagant pad by handling or
non sterile container.
pH may be falsely elevated if the urine is stale.
Some medication can affect some of the reagents
on the strips (e.g. cephalosporins; L-dopa; high levels
of salicylates; chlorhexadine; ferrous sulphate)
Strips out of date.
Vegetarians may have a urine pH >8.
Visual significance of urinalysis
Colour: The colour and clarity of the urine has significant
implications and should always be noted. The colour of
normal urine varies with its concentration, from deep
yellow to almost clear. In disease, the colour may be
abnormal due to excretion of the endogenous pigments
as well as drugs and their metabolites.
Odour: Odour in the urine of patients who have a urinary
tract infection, is often due to the urea-splitting
organisms. This makes it smell ammonia. The presence of
urinary ketones, as in diabetic ketoacidosis, leads to an
acetone smell. The presence of malodorous urine does
not indicate the presence of infection and does not
negate the need for testing.
Clinical significance of test
results
Glucose - is found when its concentration in
plasma exceed the renal threshold (may
indicate diabetes)
Bilirubin/urobilinogen – indicates an excess in
the plasma. Commonest cause of positive
results is liver cell injury e.g. hepatitis,
paracetamol overdose, late-stage cirrhosis.
Ketones – due to excessive breakdown of body
fat. Common in fasting, may indicate low
carbohydrate diet, vomiting & fever, present in
starvation
Clinical significance of test
results (cont.)
Specific gravity – a measure of solute concentration.
High values can be found in dehydration. Low
values found in high fluid intake. Diabetes insipidus;
chronic renal failure; hypercalcaemia;
hypokalaemia.
Blood – menstruation, kidney disorders; urinary tract
disorders (e.g. tumours, prostatic enlargement).
pH – high values - commonest cause of high vales is
stale urine; large intake of antacids;UTI with
ammonia forming organisms. Low values – acidosis
(diabetic & lactic); starvation; potassium depletion.
Clinical significance of test
results (cont.)
Protein – excess albumen in the urine is unusually due
increased permeability in the glomeruli. Positive results
in acute and chronic kidney disease, pre-eclampsia.
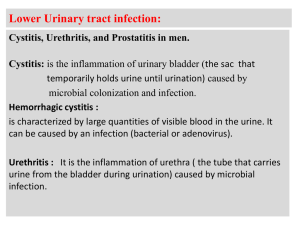
Nitrite – UTI – most of the organisms which infect the
urinary tract contains an enzyme that convers nitrate
(normally found in urine) to nitrite which is not found in
urine in the absence of infection. Some organisms do
not convert nitrate to nitrite (false negative).
Leucocytes – leucocytes enter inflamed tissue from
the blood and are shed into the urine. UTI is
commonest cause of positive results.
UTI testing pathway
Urine sample
clear
Test with reagent
strip
Obviously infected
Send for C&S /
treat
Visual appearance
If all Negativenitrite, leucocytes,
blood, protein discard
If any Positive –
nitrates,
leucocytes, blood,
protein = UTI
Any questions?