Phil Riley Presentation
advertisement
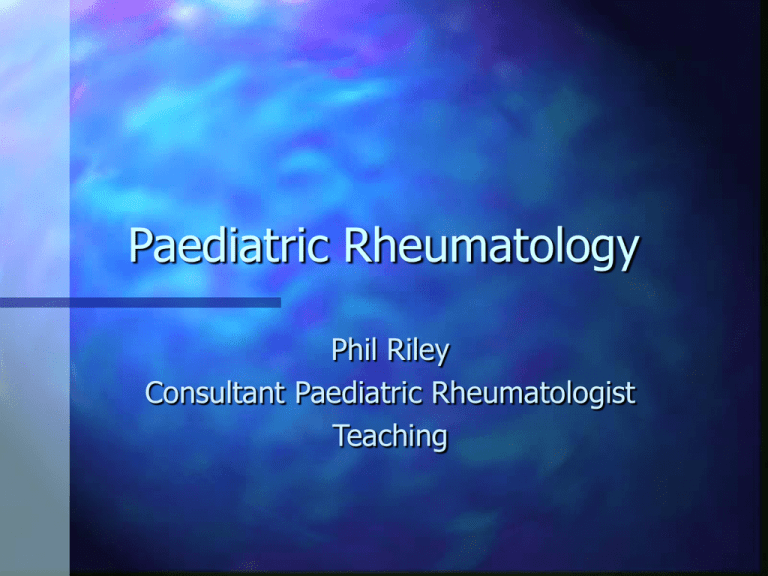
Paediatric Rheumatology Phil Riley Consultant Paediatric Rheumatologist Teaching Introduction Musculoskeletal pain common in childhood Wide range of diagnoses -benign to malignant JIA- early recognition and appropriate treatment prevents damage JIA- Multidisciplinary team Differential Diagnosis Inflammatory Mechanical Psychological Differential DiagnosisInflammatory Reactive Infection Inflammatory disease Systemic disease Malignancy Irritable hip Differential DiagnosisMechanical Trauma-accidental and NAI Hypermobility Osteochondritides Degenerative disorders Haematological Metabolic Tumours- benign and malignant DifferentialPsychogenic Fibromyalgia Functional illness Reflex Sympathetic Dystrophy Juvenile Idiopathic Arthritis Unknown aetiology Genetic predisposition incidence 1 per 10,000 prevalence 1 per 1,000 Disease Course 50% still active after 25 years X-ray Joint damage by 2.6 years Increased mortality Increased morbidity-Physical -Growth -Psychological -Social Classification of Juvenile Arthritis <16 years >6 weeks arthritis Subtypes classified for first 6 months Subtypes Oligoarthritis -persistent -extended Polyarthritis (RF negative) Polyarthritis (RF positive) systemic 1-4 >=5 >=5 Investigations-JIA ANA- Antinuclear antibody Inflammatory markers- CRP,ESR FBC- Anaemia of chronic disease x-ray -loss of joint space, erosions and carpal bone overcrowding MRI- synovitis (gadolinium enhanced) Uveitis Chronic anterior uveitis Often Asymptomatic Young,female, oligoarthritis, positive ANA (30%) Polyarthritis (5%) systemic(rare) Slit lamp 3-6 monthly for 7 years Subtypes Systemic Arthritis -Rash -temp over 2 weeks -with/without arthritis -with/without serositis -hepatosplenomegaly, lymphadenopathy JIA systemic rash Systemic JIA Quotidian fever Systemic JIA Macrophage Activation Syndrome(MAS) -Bleeding, purpura, bruising -Nodes,liver,spleen -FBC,ESR -PT,APTT, FDP - Fibrinogen,clotting factors Bone Marrow IV steroids,Cyclosporin Subtypes Enthesitis-related arthritis -HLA B27 Psoriatic Arthritis Other Treatment Options NSAIDs Steroids Joint injections Methotrexate Sulphasalazine Ciclosporin TNF drugs Autologous stem cell transplantation Questions Oligoarthritis ANA pos normal slightly raised ESR,CRP NSAIDS Joint injection Ophthalmology referral Rehab/MDT Questions Polyarthritis ANA positive or negative Rh factor positive or negative very raised ESR,CRP Steroids Methotrexate Eyes Rehab/MDT Questions Systemic Rash Quotidian fever NSAIDS Steroids Methotrexate Macrophage Activation Syndrome Treatment Concepts Early Monitoring Multidisciplinary Treatment continued Physiotherapy restore function improve muscle strength splints/serial casts Occupational therapy Psychology Spotter Butterfly Rash Spotter Buttterfly Spotter Raynaud’s phenomenon SLE- Diagnostic/ WHO classification criteria(4 of 11) Malar rash(butterfly) Discoid lupus rash Photosensitivity Oral/nasal mucosal ulceration Non-erosive arthritis nephritis -proteinuria/cellular casts SLE-Diagnostic/WHO classification(4 of 11) Encephalopathy-seizures/psychosis Pleuritis/pericarditis Haematological -lymphopaemia -thrombocytopaenia positive immunoserology -anti ds-DNA ANA positive SLE- clinical features Constitutional - fever/malaise/weight loss Cutaneous rash/photosensitivity/alopecia/mouth ulcers Musculoskeletal poly-arthritis/arthralgia tenosynovitis myopathy avascular necrosis SLE-Clinical features Vascular lupus crisis/Raynaud’s/livedo Cardiac pericarditis/myocarditis/endocarditis Pulmonary pleuritis/pneumonitis/haemorrhage SLE-lab features FBC- low platelets - low lymphocytes Inflammatory markers- high ESR, normal CRP ANA- very high ie >1:2560 DsDNA- high C3,C4- low Spotter Neonatal lupus Spotter Neonatal Lupus Neonatal lupus Maternal autoantibody transmission Cong heart block (Ro/La) - 50% Cutaneous neonatal lupus - 37% Hepatic/GI tract - 8% Haematologic -6% Neurologic and pulmonary -1% Spotter Heliotrope Rash Spotter Gottrons papules Spotter Calcinosis Spotter Capillaroscopy Abnormal “bushy” Thickening and dropout Definition of Juvenile Dermatomyositis(JDM) limb-girdle and anterior neck flexor weakness Muscle biopsy Muscle enzyme increase EMG Dermatological features JDM - clinical features Proximal weakness Vasculopathy Heliotrope facial rash Gottrons papules Raised CK/LDH/AST/ALT MR scan/muscle biopsy Multi-organ occasionally JDM - treatment Steroids pulse iv oral tapering Methotrexate Cyclosporin/Immunoglobulin/Cyclophos phamide/Anti TNF Physio/Rehab Spotter en coup de sabre Spotter Sclerodactly Scleroderma in children Systemic sclerosis limited cutaneous/CREST diffuse Localised linear scleroderma (en coup de sabre,morphoea) Questions Q1 Q1 Q2 Q3 Q4 Q5 Q6 Q7 Q8 Q9 Q10 Q11 Q12 Q13 Q14 Q15 Q16 Q17