Delivery of CBT-I to an Underserved Population in Primary Care
Session I5-Tapas
Saturday, October 29, 2011
Implementing Cognitive Behavioral
Therapy for Insomnia in Primary
Care
Christina O. Nash, M.S. & Jacqueline D. Kloss, Ph.D.
Department of Psychology
Drexel University, Philadelphia
Objectives
1.
2.
3.
Briefly review literature on CBT-I in
Primary Care settings
Highlight the additional challenges via a case vignette while delivering CBT-I in light of current research
Identify areas for clinical discussion and pose research questions for future investigation
Prevalence of Insomnia in Primary Care
Widely recognized that primary care settings serve as the
“front lines” for recognizing and initiating treatment for insomnia
Many individuals with Primary Insomnia seek out help with their general practitioner(Aikens & Rouse, 2005)
50% of individuals in primary care complain of insomnia, making insomnia one of the most common complaints at general practitioner offices (Schochat, Umphress, Israel, &
Ancoli-Israel, 1999; NHLB Working Group on Insomnia)
Among a sample of 1,935 primary care patients, one third met criteria for insomnia, more than 50% reported excessive daytime sleepiness (Alattar, Harringon, Mitchell & Sloane,
2007).
Obstacles and Challenges to the Delivery of
CBT-I in PC Settings
◦ Assessment and recognition of insomnia; differential diagnosis
◦ Fast-paced setting, yet need for integrated care and collaborative relationships with behavioral health consultants
◦ Managing insomnia given a complex health picture and understanding its comorbidites (e.g., chronic health conditions)
◦ Despite efficacy of CBT and patient preference for nonpharmacological approaches, prescription medications are most commonly administered (Chesson, et al, 1999) and
CBT-I is underutilized (Morin, 1999; Espie, 1998)
◦ Health Care Providers are untrained in sleep medicine
Additional Challenges of Delivering CBT-I to
Underserved Populations
◦ Chronic health concerns in general are even more pronounced in lower
SES groups. For example, disparities documented in cancer, diabetes, cardiovascular disease, HIV, psychiatric comorbidities among underserved (Winkelby, Jatulis, Frank & Fortmann, 1992)
◦ Sleep quality is inversely related to income, unemployment, education
(Moore, Adler, Williams, Jackson, 2002; Ford and Kamerow, 1989)
◦ Individuals with lower SES as measured by education level were more likely to experience insomnia while controlling for gender, age, and ethnicity (Gellis et al., 2005) and those who have dropped out of high school demonstrated the greatest impairments due to insomnia
◦ Paucity of research on interrelationships between race, ethnicity, SES and insomnia; For example, perhaps poor sleep may account for the relationship between low SES and health disparities (Arber, Bote, &
Meadows, 2009; Cauter & Spiegel, 1999)
◦ Shift work more common among low SES, and linked to poorer sleep quality and poorer health outcomes (Cauter & Spiegel, 1999)
Research Background to CBT-I Delivery to Underserved in PC Settings
A number of studies have initiated abbreviated CBT implementation in PC settings with success (e.g, Edinger &
Sampson, 2003; Goodie et al., 2009; Hyrshko-Mullen et al,
2000; and some with primary care nurses (e.g., Espie et al,
2001; 2007; Germain et al., 2006)
However, to our knowledge, little, if any research has been conducted to examine Sleep Disorders, and specifically insomnia, among underserved community primary care patients
One study, McCrae et al. (2007) a 2-day workshop delivered by service providers (mental health counselor, a provisionally licensed counselor, and social worker) yielded significant improvement in a rural setting with elderly population
Translating CBT-I Research to Practice among Underserved Populations
How do we translate and deliver our well-established CBT-I approaches not only within a fast-paced PC setting in an abbreviated modality with care professionals who likely have limited sleep knowledge, but also to populations with complex health histories, impoverished environments, and with limited resources?
Observations from Community Health Center
Ethnicity/Race: Latino and African-American patients
Over 98% of patients are 200% below the poverty line
Potential for comorbidity
◦ 24.3% of patients met criteria for Major Depressive Disorder (MDD)
◦ 26% met criteria for Generalized Anxiety Disorder (GAD)
◦ 28.5% met criteria for Post-traumatic Stress Disorder (PTSD)
◦ In a study of a sample of 288 patients conducted in 2003, 46% of patients met criteria for a DSM-IV-TR diagnosis, 14% met criteria for 2 diagnoses, and 11% met criteria for 3 diagnoses.
Of 9057 adult patients seen during the last year, 158 were diagnosed with
Psychophysiological Insomnia, 2 with Insomnia, Unspecified
◦ Over half of these patients reported symptoms of insomnia during their medical visit
◦ 120 of these patients with diagnosed insomnia are currently prescribed
Zolpidem (i.e., Ambien)
◦ Of 9057 patients, 125 were seen by Behavioral Health for screening and/or consultation
Observations from the Community
Health Center
Language barriers
Literacy
Legal status
Unemployment/Lack of a daytime routine
Patients sleeping in shelters/Homeless
Impoverished sleep environments may lead to poor sleep hygiene (e.g., noise, fear, bed availability, curtains, temperature)
Limited access to sleep education and sleep specialists
Case Vignette
Unemployed and lacks a daytime routine
History of
Domestic
Violence Diagnosed with
MDD, GAD &
PTSD
Safety Concerns in Neighborhood
Rosa
Chronic
Medical
Conditions
Did not graduate high school
One bed for four people
English as a second language
Nightmares
Treatment Implementation
Behavioral Health Consultation Delivery of CBT-I
Consult 1 “Warm-handoff” by PCP. Gathered patient history and provided psychoeducation on sleep hygiene. Sleep diaries were distributed.
Consult 2 Assess sleep diaries and implement Stimulus Control procedures. Progressive muscle relaxation strategies are introduced to help patient cope with her anxiety at bedtime.
Consult 3
Consult 4
Consult 5
Consult 6
Consult 7
Consult 8
Patient reports difficulty with Stimulus Control. Strategies are discussed and implementation is encouraged. PMR is reviewed.
Patient reports she is engaging in stimulus control and has been “sleeping better.” Sleep
Restriction is introduced and the continuation of Stimulus Control strategies is recommended.
Patient reports she has been having difficulty with Sleep Restriction and her sleep restriction schedule is reviewed.
Patient is a “no show” for her scheduled appointment.
Patient reports that she has been sleeping with less nighttime awakenings and has been falling asleep in less than 30 minutes. She is encouraged to continue utilizing CBT-I strategies.
Patient’s self-report of insomnia severity is below the threshold for insomnia. Patient wishes to discontinue behavioral health consultation at this time and promises to contact DVCH if she is having sleep difficulties again. She is encouraged to continue engaging in CBT-I.
Rosa Sleep Diary Data*
SOL
1.5 hrs
WASO
2.5 hrs
TST
4hrs Consult 1
(Baseline)
Consult 2
Consult 3
Consult 4
Consult 5
Consult 6
Consult 7
Consult 8
1.25hrs
Missing
1hr
Missing
45 min
40 min
25 min
2.5hrs
Missing
2hrs
Missing
30 min
45 min
30 min
4hrs
Missing
5.75hrs
Missing
6.25hrs
7.25 hrs
7.25 hrs
*Weekly Averages
TIB
8 hrs
7.75 hrs
Missing
7.75 hrs
Missing
6.65hrs
7.65hrs
8.70hrs
Insomnia Severity
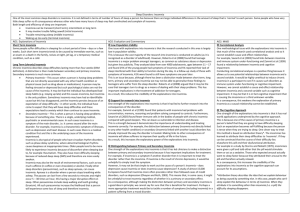
Practices and Pitfalls of CBT-I in the
Community Health Center
Method of Treatment
Delivery
“Practices” “Pitfalls”
Self-administered CBT “Cold calls” vs. “warm hand-offs” Having proper screening devices; collaborative relationships; knowledge and training; efficacy of self-help treatments?
Language barriers and Literacy
Small Group manualized brief
CBT delivered by a trained therapist
Where available, can be ideal, e.g., graduate student training model
Limited resources; rural settings; adequate training care providers, consulting BSM specialists
Individual or small group CBT delivered by a graduate psychologist
Availability of these training models
Individual, tailored CBT delivered by a clinical psychologist or
Expert CBT-I delivered by a BSM
Specialist
Limited research on efficacy of abbreviated models and limited availability
Need for supervision, BSM specialist consultation; need research on efficacy; volume outweighs staff
Cost, volume, accessibility;
Follow-up
Adapted from Espie’s Stepped Care Model (2009)
Future Research and Clinical Considerations
◦ Epidemiological studies on the links between SES and insomnia (e.g., understanding the mechanisms that link insomnia and SES, education, and health); studies on incidence, prevalence, and presentation/manifestation of insomnia
◦ Additional efficacy studies on abbreviated CBT approaches specifically with underserved populations (e.g., in rural settings, at community health centers, varied educational levels); Does one size fit all?
◦ Psychometrically sound screening and assessment measures (e.g.,
Kroenke et al, 1999; PHQ-9)
◦ How effectively can “in house” care providers deliver CBT-I? Under what conditions? How do we best access BSM specialists and provide adequate supervision and training?
◦ How do we foster collaborative relationships into an integrative care system with the use of behavioral health consultants and/or BSMtrained practitioners?
◦ Consider complex comorbidities (physical and mental health problems)
◦ Enhance decision-making about pharmacotherapy
Where do we go from here?
Stepped Care Model (Espie, 2009)
Meta-analyses demonstrated self-help tools (books, internet) to have a small to moderate effect size (Straten & Cuijpers,
2009)
Tele-health, Internet and Telephone
Consultations (e.g., Vincent& Lewycky,
2009; Bastien et al, 2004)
Group CBT-I
Implementation of Training Models
References
Alattar, M., Harrington, J.J., Mitchell, M.,, & Sloane, P. (2007). Sleep problems in primary care: a North Carolina family practice research network (NC-FP-RN) study. JABFM, 20, 365-374.
Arber, S., Bote, M. & Meadows, R. (2009). Gender and socio-economic patterning of self-reported sleep problems in
Britain. Social Science & Medicine, 68, 281-289.
Espie, C.A. (2009). “Stepped care”: a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. SLEEP, 32(12), 1549-1558.
Espie, C.A., Inglis, S.J., Tessier, S., & Harvey, L. (2001). The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: implementation and evaluation of a sleep clinic in general practice. Behaviour Research and Therapy, 39, 45-60.
Ford, D.E., & Kamerow, K.B. (1989). Epidemiologic study of sleep disturbances and psychiatric disorders. Journal of the
American Medical Association, 262, 1479-1484.
Gellis, L. A., Lichstein, K. L., Scarinci, I.C., Durrence, H.H., Taylor, D.J., & Bush, A.J. (2005). Socioeconomic status and insomnia. Journal of Abnormal Psychology, 114(1), 111-118.
Germain, A., Moul, D.E., Franzen, P.L., Miewald, J.M., Reynolds, C.F., Monk, T.H., & Buysse, D.J. (2006). Effects of a brief behavioral treatment for late-life insomnia: preliminary findings. Journal of Clinical Sleep Medicine, 2(4), 403-406.
Goodie, J.L. , Isler, W.C., Hunter, C., & Peterson, A.L. (2009). Using behavioral health consultants to treat insomnia in primary care: a clinical case series. Journal of Clinical Psychology, 65(3), 294-304.
McCrae, C.S., McGovern, R., Lukefahr, R., & Stripling, A.M. (2007). Research evaluating brief behavioral sleep treatments for rural elderly (RESTORE): a preliminary examination of effectiveness.
Moore, J.P., Adler, N.E., Williams, D.R., & Jackson, J.S. (2002). Socioeconomic status and health. The role of sleep.
Psychosomatic Medicine, 64, 337-344.
Winkelby, M.A., Jatulis, D.E., Frank, E. & Fortmann, S.P. (1992). Socioeconomic status and health: How education, income, and occupation contribute to risk factors of cardiovascular disease. Journal of Public Health, 82(6), 816-820.