Skin
advertisement

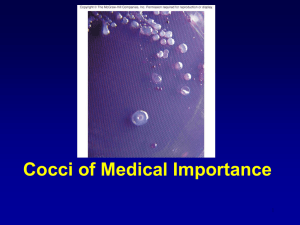
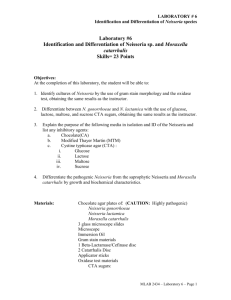
Pyogenic Coccus The Staphylococci Morphology & Identification Gram positive Facultative anaerobes Grape like-clusters Catalase positive Major components of normal flora skin nose Gram Positive cocci - staphylococci Pus Catalase test(过氧化氢酶) (-) (+) Pathogenesis & Immunity of Staphylococcus aureus Antigenic Structure Protein A inhibits phagocytosis Fc receptor immunoglobulin PHAGOCYTE Protein A BACTERIUM Toxins & Enzymes • Catalase • Coagulase • Hyaluronidase and Lipase • • • • • Hemolysin or sphingomyelinase C Leukocidin Exfoliative Toxin Toxic Shock Syndrome Toxin (superantigen) Enterotoxins Pathogenesis Pathogenesis of staphylococcal infections Stye:麦粒肿 Carbuncle:痈 Impetigo:脓疱疮 Infections associated with indwelling devices Superantigens and the non-specific stimulation of T cells Clinical Findings- Suppurative • A. (Skin) Furuncle; Protein A, Leukocidin, Hemolysin Stye; lipase Impetigo; contagious Epidermal necrolysis Exfoliative Dermatitis (6,7,8); Exfoliative toxin Mastitis Abscess (deep tissue); granulation; coagulase, hyaluronidase (burn, wound) • B. Systemic : Bactermia (from abscess, wound, burn) , Osteomyelitis (tibia) ,Pneumonia Clinical Findings- Food poisoning • not a human infection • food contaminated from humans – growth – enterotoxin • onset and recovery both occur within few hours • Vomiting/ nausea/ diarrhea/ abdominal /pain Toxic shock syndrome • fever • scarlatinifor m rash • desquamatio n • vomiting • diarrhea S. aureus • babies –scalded skin syndrome * exfoliatin Pseudomembranous Colitis Laboratory • • • 1. 2. 3. • • • A. Direct examination; Gram Stain B. Primary media; BAP C. Differential Tests. Mannitol Salts Coagulase DNase D. Phage typing E. Antibiotic Sensitivity (plasmid, B lactamase) penicillin /methicillin/vancomycin Summary Figure (Identification Scheme) Note: Strep. viridans are alpha hemolytic and negative for all the tests below GRAM POSITIVE COCCI Catalase Streptococcus (pairs & chains) + Staphylococcus (Clusters) Coagulase + S. aureus &hemolytic mannitol yellow - Hemolysis • S. epidermidis nonhem olytic (usua lly) mannitol (2) white • BETA: Bacitracin S .pyogenes (group A) + CAMP/Hippurate + S. agalactiae (group B) ALPHA: Optochin/Bile Solubility GAMMA: Bile Es culin + S. pneumoniae + 6.5% NaCl + Group D* Enterococcus Bile Esc ulin NaCl Group D* + 6.5% Non-Enterococcus (*can also be beta or alpha hemolytic) S. aureus on BAP Mannitol Salt Agar DNase test 0.1% Toluidine blue O (+): Pink 1N HCl (+) : S. aureus on potassium tellurite agar Lysostaphin test Staphylococcus Micrococcus API STAPH Kit Staphylococcus epidermidis • major component skin flora • opportunistic infections – less common than S.aureus • nosocomial infections – heart valves • Identification – Non-hemolytic (sheep blood agar) – Does not ferment mannitol – Non-pigmented – Coagulase-negative Staphylococcus saprophyticus • urinary tract infections • coagulase-negative – not differentiated from S. epidermidis The Streptococcus Streptococcus Morphology & Identification • • • • facultative anaerobe Gram-positive Chains or pairs Catalase negative (staphylococci are catalase positive) Cell surface structure of S pyogenes and extracellular substances S. pyogenes lipoteichoic acid F-protein fibronectin epithelial cells M protein • major target – natural immunity • strain variation – antigenicity • re-infection – occurs with different strain M protein IMMUNE Complement IgG r r r M protein NON-IMMUNE peptidoglycan fibrinogen r r r Capsules • Anti-phagocytic – mucoid strains • Streptococci • Lancefield groups *one or more species per group *surface antigens groupable streptococci • A, B and D –most important • C, G, F –rare Non-groupable • S. pneumoniae –pneumonia • viridans streptococci –e.g. S. mutans * dental caries Toxins & Enzymes Hemolysis alpha beta gamma Classofication of Streptococci of Particular Medical Interest Pathogenesis of S pyogenes infections. • Group A streptococcal infections affect all ages peak incidence at 5-15 years of age S. pyogenes -suppurative • non-invasive – pharyngitis – skin infection, impetigo • invasive bacteremia – toxic shock-like syndrome – "flesh eating" bacteria – pyrogenic toxin Pyrogenic toxin • superantigen • T cell mitogen • activates immune system Scarlet fever • rash • erythrogenic toxin non-suppurative • rheumatic fever – inflammatory disease – life threatening – chronic sequalae • fever • heart • joints • rheumatic NOT rheumatoid arthritis Rheumatic fever -etiology M protein – cross-reacts heart myosin – autoimmunity cell wall antigens – poorly digested in vivo – persist indefinitely Rheumatic fever Acute glomerulonephritis • immune complex disease of kidney Group B streptococcus • neonatal meningitis • septicemia • transmission – vaginal flora Group B streptococcus identification • hemolysis • hippurate hydrolysis • CAMP reaction – increases hemolysis of S. aureus Group D streptococcus • Growth on bile esculin agar – black precipitate • 6.5% saline • grow – enterococci • no growth – non-enterococci Enterococci • distantly related to other streptococci • genus Enterococcus • gut flora – urinary tract infection • fecal contamination – opportunistic infections • particularly endocarditis • most common E. (S.) faecalis Enterococci • resistant to many antibiotics – including vancomycin • terminal D-ala replaced by D-lactate Viridans streptococci • • • • • • diverse species oral dental caries hemolytic and negative for other tests non-groupable. includes S. mutans – endocarditis – tooth extraction Diagnostic Laboratory Test Post-infectious diagnosis (serology) • antibodies to streptolysin O • important if delayed clinical sequelae occur Serotyping M T R S. pneumoniae - diplococci S. pneumoniae Virulence factors • a. capsule: It is antiphagocytic, inhibiting entrapment and phagocytosis where type-specific opsonic antibody is absent. Non-capsulate mutants are avirulent in experimental animals. • b. pneumolysin: It suppresses phagocytic oxidative burst. It is a membrane-damaging toxin. Thus it can destroys red blood cells and possibly ciliated epithelial cells. • c. Surface protein adhesinand secretory IgA protease: The biologic effects are to help S.pneumoniae for the colonization and migration. • d.Teichoic acid and the Peptidoglycan fragment, phosphorylchorine : They can mediate the mobilization of inflammatory cells to the focus of infection and cause the tissue Capsule • prominent – virulent strains • anti-phagocytic • carbohydrate antigens – vary among strains • immunity – serotype specific • vaccine contains multiple serotypes • only for susceptible population clinic finding • leading cause pneumonia – particularly young and old – after damage to upper respiratory tract *e.g. following viral infection • bacteremia • meningitis • middle ear infections (otitis media) (-) (+) (Bile solubility test) Autolysis - identification autolysin teichoic acid -choline peptidoglycan cell membrane lipoteichoic acid Bile Identification Not optochin sensitive optochin sensitive Quellung reaction • using antisera • capsule "fixed" • visible microscopically Streptex antiserum Latex agglutination - streptococci Summary Figure (Identification Scheme) Note: Strep. viridans are alpha hemolytic and negative for all the tests below GRAM POSITIVE COCCI Catalase Streptococcus (pairs & chains) + Staphylococcus (Clusters) Coagulase + S. aureus &hemolytic mannitol yellow - Hemolysis • S. epidermidis nonhem olytic (usua lly) mannitol (2) white • BETA: Bacitracin S .pyogenes (group A) + CAMP/Hippurate + S. agalactiae (group B) ALPHA: Optochin/Bile Solubility GAMMA: Bile Es culin + S. pneumoniae + 6.5% NaCl + Group D* Enterococcus Bile Esc ulin NaCl Group D* + 6.5% Non-Enterococcus (*can also be beta or alpha hemolytic) Prevention and Treatment • Immunity ; 14 capsule types mixed vaccine • Most strains susceptible to penicillin , but resistance is common NEISSERIA Neisseria gonorrhoeae Neisseria • Gram negative • diplococci (pairs of cocci) • oxidase positive • culture • Thayer Martin. – selective – chocolate agar * heated blood (brown) N. meningitidis N. gonorrhoeae Virulence Factors Similar, but – Differences in utilization LPS LPS Capsule IgA protease Hemolysin IgA protease PILI Opacity (OPA) proteins Outer Membrane Proteins PILI Opacity (OPA) proteins Outer Membrane Proteins X NO capsule NO hemolysin N. gonorrhoeae the "gonococcus" • After 2-14 days •Found only in man • Gonorrhea: second most common venereal disease Neisseria gonorrhoeae Gram stain of pure culture Urethral exudate Using the Gram stain in patient specimens, the organisms are most often observed in polymorphonuclear leukocytes Neisseria gonorrhoeae Neisseria gonorrhoeae Pili = key in anchorage of organisms to mucosal epithelium. Nonpiliated gonococci are avirulent OUTER MEMBRANE PROTEINS Porin proteins (Por) = prevent phagolysosome fusion & allow intracellular survival [ also called protein I] Opacity proteins (Opa) = binding of organisms to epithelium [also called protein II] Reduction-modifiable proteins (Rmp) = protection against bactericidal antibodies [ also called protein III] Neisseria gonorrhoeae Symptomatic infections are notably PURULENT Urethritis Neisseria gonorrhoeae Symptomatic infections are notably PURULENT Bartholin’s Duct Neisseria gonorrhoeae Purulent conjunctivitis Ophthalmia neonatorum Infection in newborns during vaginal delivery Neisseria gonorrhoeae Disseminated gonococcal infection (DGI). Fever, polyarthritis (or monoarticular septic arthritis), and/or dermatitis (pustules on a hemorrhagic base). Smear • polymorphonuclear cell • Gram negative cocci many in cells • Culture Antibiotic therapy • lactamase-resistant cephalosporin – e.g. ceftriaxone • resistant strains – common – produce lactamases – destroy penicillin N. meningitidis (the "meningococcus") N. meningitidis • resides in man only • usually sporadic cases – mostly young children • outbreaks – adults – crowded conditions * e.g. army barracks Neisseria meningitidis upper respiratory tract infection – adhesion pili bloodstream brain Meningococcal meninigitis • 1-4 days • Second most common meningitis – pneumococcus, most common • Fatal if untreated • Responds well to antibiotic therapy – penicillin Laboratory Diagnosis • spinal fluid – Gram negative diplococci within polymorphonuclear cells – meningococcal antigens • Culture – Thayer Martin agar Prevention - Capsule • capsule – inhibit phagocytosis • anti-capsular antibodies – stop infection • antigenic variation – serogroups • vaccine – multiple serogroups