Paediatric History Taking & Examination STEPP
advertisement

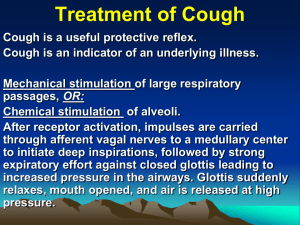
Paediatric History Taking & Examination STEPP Teaching, Dee Aswani, SpR Overview of Session Principles of Paediatric History Taking Practical Exercise Examination Tips Baby Checks A smart mother makes often a better diagnosis than a poor doctor. August Bier (1861–1949) Differences to adult practice & General Principles Children are not small adults LISTEN CAREFULLY to what the mother is telling you - she knows her child best and intuitively knows when something is wrong. She is RIGHT unless proven otherwise Useful to quote verbatim, but ask to define terms for eg - what does ‘diarrhoea’ actually mean? Additional important features of the history Always consider CHILD PROTECTION issues Components of History Presenting complaint History of presenting complaint Past medical history Incl feeding history & growth Birth History Developmental History Immunisation History Drug History Family History Social History Inadequate History Cough x 3 days Off feeds x 2 days Wheeze x 1 day Temperature x 1 Vomit x 2 70% of paediatric diagnoses will be obtained by history alone Peter, age 7 years, referred by GP “difficulty breathing” History of presenting complaint Coughing since started at school 2 years ago ‘always has a cough’ Worse since last night teatime Vomited x 1 last night, cough induced No fever Has been breathless Breathing sounds noisy Cough sounds productive Complaining of tummy ache Cough wakes him at night, often needs a glass of water to settle down Coughs approx 5 nights out of 7 Tired and difficult to wake in the morning Missing a lot of school Difficulty keeping up with peers at PE General lack of energy, prefers to sit and watch telly rather than playing outside with friends, complains that ‘chest hurts’ No history of choking or foreign body Came back from holiday in Turkey a week ago Still in same school trousers as in reception, one of the smallest in class Good appetite Past Medical History One previous A&E attendance - was wheezy, had ‘steam medicine’ then went home Frequent chest infections treated by GP with antibiotics No operations or admissions Has mild eczema Birth History Born at 34 weeks Emergency Section , 4lb 8oz, foetal distress Spontaneous labour and PROM Pregnancy and scans fine Was on SCBU for 3 weeks Needed CPAP for 1 day and then some oxygen for a while No oxygen when went home Developmental History Smiled at 10 weeks Sat at 6 months Never crawled Walked at 13 months Started talking around 18 months No problems with hearing or vision Average progress at school Immunisation History ‘up to date’ didn’t have MMR - cousin with autism Medication Oilatum in bath for eczema allergic to Penicillin had it when 2 years and ‘was sick’ Tixylix Family History Dad got eczema and hay fever Maternal grandma has diabetes Paternal Grandfather had TB Mum and Dad separated Younger 2 year old brother also has eczema Mum works in retail. Suffers with depression No consanguinuity Social History 2 Pet cats at home Mum smokes “outside” Dad also smokes Goes to a childminders 3 times a week Child spends every other weekend at Dad’s house Examination General Principles & Tips Get down to their level A lot of information can be gained by INSPECTION alone, before you lay an hand on the patient Beware of asking the child’s permission Know a conversation topic / latest craze / TV characters / films relating to different age groups Examination needs to involve play and be opportunistic but thorough Keep Mum close at hand and in child’s view or reach Keep child in the position in which they are comfortable. No need to lie them down unless you have to children are very vulnerable in this position Save the nasty things to the end so that you don’t lose trust (eg ENT) Baby checks To assess general condition To establish normality To detect major abnormalities Useful in finding eye, hip and heart problems Read Mum’s notes first Pregnancy history Paediatric Alerts Delivery notes Ask Mum if any concerns Family History Who does baby look like? OBSERVATION Appearance / Dysmorphia Alert / Drowsy Colour - anaemia / jaundice Bruising Posture Birth Marks HEAD Shape of skull - moulding, sutures OFC Fontanelles Eyes and ears Mouth - look and feel for cleft Range of neck movements RESPIRATORY SYSTEM Respiratory distress or increased work of breathing CARDIOVASCULAR SYSTEM Pulses including femorals Heart sounds Oxygen saturation - post-ductal ABDOMEN Shape Palpation - masses BO / BNO in first 24 hours Genitalia / PU HIPS Barlow /Ortolani manouvres LIMBS Position - talipes Movement Palmar creases NEUROLOGICAL SYSTEM Tone Posture Primitive reflexes Spine EYES Red reflexes Hip Examination Ortolani Barlow Primitive Reflexes SUMMARY Good Paediatric history taking needs to be through and takes practice 70% of diagnoses can be made on the history alone ALWAYS listen to the mother Children are quite often unco-operative and examinations can be difficult Be prepared to PLAY Children will respond much better to you if you actually LIKE them