AWOtherapeutics
advertisement
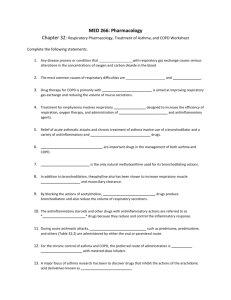
DRUG THERAPY OF AIRFLOW OBSTRUCTION PROFESSOR B J LIPWORTH • Preventers (anti-inflammatory) • Relievers (bronchodilators) THE INFLAMMATORY CASCADE Genetic predisposition + Trigger factor (e.g. viral, allergen, chemicals) Airway inflammation Mediators (e.g. histamine, leukotriene) Twitchy smooth muscle (Hyper-reactivity) • Avoidance • Anti-inflammatory - corticosteroid • Anti-leukotriene Anti-histamine • Bronchodilators - 2-agonists THE ASTHMA TREATMENT PYRAMID Oral Steroid Controller (Additive to ICS ) Preventer Reliever Theophylline Leukotriene-antagonist Long-acting 2-agonist Inhaled steroid ( Cromogylcate ?) Short-acting 2-agonist PRN Increasing severity BTS Asthma Guidelines Step 4 Step 3 Step 1 intermittent Step 2 mild persistent moderate persistent severe persistent Short-acting ß2 agonists prn Inhaled steroids Add on LABA Add on LTRA/Theo ANTI-INFLAMMATORY: CORTICOSTEROIDS • Used in asthma and COPD • Oral steroid (prednisolone) - low therapeutic ratio - only used for acute exacerbations • Inhaled steroid (beclomethasone) - higher therapeutic ratio - used for maintenance therapy • Optimise lung delivery - large volume spacer Lung deposition of HFA-BDP, fluticasone and CFC-BDP MMAD = 1.1 µm MMAD = 2.5 µm MMAD = 3.5 µm Actions of a spacer device • Avoids coordination problems with pMDI • Reduces oropharyngeal and laryngeal side effects • Reduces systemic absorption from swallowed fraction • Acts a holding chamber for aerosol • Reduces particle size and velocity • Improves lung deposition ANTI-INFLAMMATORY: CROMONES • Only used in asthma (eg Cromoglycate) • Mast cell stabiliser - weak anti-inflammatory cf steroids • Cromoglycate effective in atopic children (exercise asthma) • Inhaled route only (compliance with QID dosing ) • No longer used due to poor efficacy ANTI-INFLAMMATORY: LEUKOTRIENE RECEPTOR ANTAGONISTS • Only used in asthma: bronchodilator + anti-inflammatory • Montelukast - oral route,once daily, high therapeutic ratio • Less potent anti-inflammatory than inhaled steroid • 2nd line: complimenatary non steroidal ant-inflammatory additive to inhaled steroid • Effective in exercise induced asthma • Also effective in allergic rhinitis ( with anti-histamine ) ANTI-INFLAMMATORY: ANTIHISTAMINES • H1 receptor antagonists • Oral route • Only of value when known allergenic trigger (e.g. HDM ,pollen or cat) -ie in atopic asthma • 1st generation :Chlorpheniramine-sedative • 2nd generation: Cetirizine,Loratadine-non sedative • 3rd generation: Levocetirizine,Desloratadine - non sedative • More effective in allergic rhinitis than asthma • Additive effects when given together with leukotreine antagonist ANTI-INFLMMATORY Anti-IgE • Anti-IgE monoclonal antibody : Omalizumab (Xolair) • Omalizumab inhibits the binding to the high-affinity IgE receptor and inhibit mediator release from basophils and mast cells . • Injection every 2-4 weeks . • For patients with severe persistent allergic asthma despite max therapy –ie step 5 . • Very expensive . • No effect on pulmonary function but reduces exacerbations . BRONCHODILATORS: 2-AGONISTS Stimulate bronchial smooth muscle 2-receptors: cAMP Short-acting - salbutamol Long-acting – salmeterol / formoterol Combination inhalers-eg Seretide / Symbicort Used in asthma and COPD High therapeutic ratio when given by inhaled route Systemic 2 effects when given systemically or at high inhaled doses • High nebulised doses given in acute attack • • • • • • • Muscarinic (cholinergic) receptors M1-receptors enhance the cholinergic reflex M2-receptors inhibit acetylcholine release M3-receptors mediate bronchoconstriction and mucus secretion BRONCHODILATORS: ANTICHOLINERGICS • Block post junctional end plate M3 receptors • Ipratropium qid , Tiotropium od - inhaled route only - high therapeutic ratio • Used in COPD - less effective in asthma • High nebulised doses of ipratropium used in acute COPD and in acute asthma BRONCHODILATOR/ANTINFLAMMATORY :METHYLXANTHINES • Oral (Theophylline) for maintenance therapy • SR formulation useful for nocturnal dips • Used as add to inhaled steroid as complimentary non steroidal anti-inflammatory • IV (Aminophylline) for acute attacks • Non selective phosphodiesterase inhibitor (cAMP) • Adenosine antagonist • Low therapeutic ratio - P450 drug interactions (e.g. erythromycin) • Used in asthma and COPD Anti-inflammatory :PDE4 inhibitors • • • • • Roflumilast –oral tablet od Indicated for COPD only Minimal effect on FEV1 Reduces exacerbations –additive to LABA or LAMA Adverse effects : Nausea/Diarrhoea/Headache/Weight loss • ? Place in COPD guidelines as add on to ICS/LABA/LAMA Mucolytics • Oral carbocisteine , erdosteine • To reduce sputum viscosity and aide sputum expectoration [and reduce exacerbations ] in COPD • Rarely used –only as add on to other treatments TREATMENT OF CHRONIC ASTHMA • AIMS: Abolish sympt, min 2-use, normalise FEV1, reduce PEF variability, reduce exac, prevent long term airway remod • Avoid triggers • Suppress inflammatory cascade with inh steroid +/- non steroidal anti-inflamm therapy –eg theophylline ,antileukotriene ,anti-histamine • Stabilise smooth muscle with LABA –only once optimal antiinflamm therapy in place TREATMENT OF ACUTE ASTHMA • Oral prednisolone (or iv hydrocortisone ) • Nebulised high dose salbutamol, ± Neb ipratropium, ± iv aminophylline/magnesium • 60% O2 • ITU Assisted mecahnical intubated ventilation if falling PaO2 and rising PaCO2 - never use respiratory stimulant Non-pharmacological intervention: smoking cessation Never smoked or not susceptible to smoke FEV1 (% of value at age 25) 100 75 Smoked regularly and susceptible to its effects Stopped at 45 50 Disability 25 Stopped at 65 Death 0 25 50 Age (years) 75 Fletcher et al., 1977 TREATMENT OF STABLE COPD • Prevent FEV1 decline - stop smoking • Treat reversible component - Inhaled steroid - Short/Long acting beta-2 agonists - Short/Long acting anticholinergics -Theophylline • Pulm rehab • Vaccination –influenza/pneumococcal • Domiciliary O2 to prevent cor pulmonale • Venesection for polycythaemia • Lung volume reduction surgery for highly slected patients TREATMENT OF ACUTE COPD • • • • • • • Nebulised high dose salbutamol + ipratropium Oral prednisolone Antibiotic (amoxycillin) if infection 24-28% O2 Respiratory stimulant (doxapram) to improve ventilation Non invasive ventilation instead of doxapram ITU Intubated assisted ventilation only if reversible component (eg pneumonia)