01. Asthma bronchiale
advertisement

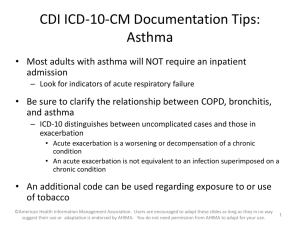
Asthma Asthma and COPD mortality Mathers, PLos Med 2006 Prevalence of astma (A) and asthmatic symptoms (B) between 1965 and 2005 in children and young adults Asthma morbidity in Hungary incidence Összes regisztrált Új betegek 2000 1000 % 000 3000 250 200 150 100 50 0 2013 2012 2011 2010 2009 2008 2007 2006 2005 2004 0 2003 % 000 prevalence 2013, OKTPI Medical history of D.B. • 30-year-old woman, school teacher • Complaints for 20 years: periods of S.O.B., particularly in the August-October period, but also during exercise (tennis), cold air exposure (skie) or under stress (exams). • Severity changes considerably time to time, with frequent attacks of wheezing, between attacks no complaints • Never smoked • Mother also had asthma Acute admission • Severe attack which responded poorly to BD drugs and inhaled CS. • Exhausted, dehydrated, very anxious • On examination: dyspneic, orthopneic, accessory muscles of respiration were active • Lungs hyperinflated, musical rhonchi in all areas • HR: 110/min with pulsus paradoxus • Sputum scant and viscid Asthma - an inflammatory disorder of the airways, characterized by periodic attacks of wheezing, shortness of breath, chest tightness, and coughing, tipically during the night and early morning. - a condition characterized by recurrent attacks of bronchoconstriction and excessive mucus production, in response to a variety of factors. - the attacks releave spontaneously or by bronchodilators - chronic inflammation results in bronchial hyperreactivity Asthma – variable nature allergenes, viruses cold weather, exercise increases Use os releaver, symptom time Asthma control decreases Exacerbation Exacerbation Prevalence 3-5% of adults and 7-10% of children. *Half of the people with asthma develop it before age 10 and most develop it before age 30. Asthma symptoms can decrease over time, especially in children. Concomittant diseases Many people with bronchial asthma have an individual and/or family history of allergies such as hay fever (allergic rhinitis) or eczema. Others have no history of allergies or evidence of allergic problems. Phenotypes Wenzel, Lancet 2006 House dust mite (Dermatophagoides pteronyssimus) Inflammatory cells Mast cell eosinophil Th2 basophil neutrophil platelet Structural cells Epithel Smooth muscle Endothel Fibroblast Nerves Mediators Histamin Leukotrienes Prostanoids PAF Kinins Adenosin Endothelins NO Cytokines Chemokines Growth factors Effects Brochospasm Plasma exsudation Mucus secretion AHR Structural changes Etiology * In sensitive individuals, asthma symptoms can be triggered by inhaled allergens (allergy triggers) such as pet dander, dust mites, cockroach allergens, pollens. * Asthma symptoms can also be triggered by respiratory infections, exercise, cold air, tobacco smoke and other pollutants, stress, food or drug allergies. * Aspirin and other non-steroidal anti-inflammatory medications (NSAID) provoke asthma in some patients. „The September epidemic” (Ontario, Canada, 2001-2004) Johnston & Sears, Thorax 2006 MODERN VIEW OF ASTHMA Allergen Macrophage Mast cell Th2 cell Mucus plug Neutrophil Eosinophil Epithelial shedding Nerve activation Subepithelial fibrosis Plasma leak Oedema Mucus Vasodilatation hypersecretion New vessels hyperplasia Sensory nerve activation Cholinergic reflex Bronchoconstriction Hypertrophy/hyperplasia Inflammatory and immune cells involved in asthma Typical pathologic features: epithel shedding + basement membrane thickening After ICS Before ICS Effect of inhaled steroid in asthma Laitinen LA, et al. J Allergy Clin Immunol 1992;90(1):32-42 Infect theory Th1 – Th2 imbalance Asztma and COPD 2 Characteristics Symptoms 1. *Most people with asthma have periodic wheezing attacks separated by symptom-free periods. *Some asthmatics have chronic shortness of breath with episodes of increased shortness of breath. *Asthma attacks can last minutes to days, and can become dangerous if the airflow becomes severely restricted Symptoms 2. Cough, Wheezing, Dyspnoe - usually begins suddenly - episodic - may be worse at night or in early morning - aggravated by exposure to cold air, by exercise, by reflux - resolves spontaneously or by bronchodilators - cough with or without sputum (dyscrinia) - breathing that requires increased work - intercostal retractions - abnormal breathing pattern: exhalation (breathing out) more than twice as long as inspiration (breathing in) Dyscrinia Symptoms 3. Emergency symptoms *extremely difficult breathing *bluish color to the lips and face *severe anxiety *rapid pulse (pulsus paradoxus) *sweating *decreased level of consciousness (severe drowsiness or confusion) during an asthma attack Signs and tests Listening to the chest (auscultation) during an episode reveals wheezing. Lung sounds are usually normal between episodes. Tests may include: *pulmonary function tests *chest X-ray *allergy testing by skin testing or serum tests (IgE) *arterial blood gas *eosinophil count Diagnostics -Lung function 1. - Between the attacks: may be normal - During the attacks: obstruction (PEF, FEV1 decreased) - Patients with - normal lung function: provocation tes - obstruction: pharmacodynamic test Metacholin provocation test bronchial hyperreactivity Pharmacodynamic test reversible obstruction Lung function 2. Provocation test *Specific provocation-allergen challenge (rarely done, can be dangeorus) inhalation causes prompt and sign. bronchoconstriction *rapid decline in FEV1: lasts: 15 min.- 1 hour *=early asthmatic reaction (EAR)=early phase response *After this phase resolves (spontaneously or with -agonist), the FEV1 reaches a level to the pre-chall. baseline. *6-24 hours after exposure to the allergen bronchoconstriction can be developed=late asthmatic response (LAR). The decline in FEV1 may be less severe. *Aspecific provocation (histamin, metacholin): *Exercise test – 6-8 min run, pre/post LF Pharmacodynamic test:baseline obstr.lung function resolved in 15 min due to inh. bronchodilatator Differencial diagnostics I. Respiratory • COPD • Large airway obstruction – Foreign body – Tumor • Pulmonary embolism • Eosinophil pneumonia • Chronic cough – – – – Bronchitis simplex Sinusitis Tracheitis Dyskinesis Non-respiratory • CHF • Gastroesophageal reflux (GERD) • Chronic cough – Drug-induced (ACE inhibitor, -blocker) Differencial diagnostics II. • • • • • • X-ray (chest, sinuses) Rhinoscopia Oesophageal pH monitoring Bronchoscopy Echocardiography Lung scintigraphy (V/Q scan) Asthma diff. dg.1./A COPD Farmacodynamic test: 61 years old man prae post FVC: 2,00 (47%)- 1,89 (44%) FEV1: 0,93 (28%)- 0,88 (26%) FRC:5,29 (150%)- 5,09 (144%) RV: 4,65 (201%)- 4,57 (198%) Raw: 6,01-6,19 (<2,24) Irreversible obstructive pulmonary disease Asthma diff. dg.1./B COPD/Emphysema Lung function 68 years old man FVC: 3,05 86% FEV1:1,03 37% VC:3,56 96% FRC:5,93 171% RV: 4,27 173% RV/TLC%: 55% DLCO: 1,6 20% Blood gas analysis pH: 7,42 pO2: 66,6 Hgmm pCO2:37,2 Hgmm Sat: 93% Asthma diff.dg 2. Tumor of big airway Asthma diff.dg 3.Heart failure Asthma severity Sympotms Day Night IV. Chronic severe III. Chronic moderate Folyamatos, naponta többször folyamatos gyakori Exercise capacity Folyamatosan korlátozott Lung function (FEV1 or PEF) FEV1 60% PEF variability30% FEV1 60-80 % Panaszok idején fizikai terhelhetőség PEF variability30% 1 hét Minden nap napi tünetek agonista minden nap II. Chronic mild Hetente többször, Nagyobb fizikai de nem minden nap terhelés köhögést és FEV1 80% bronchospazmust PEF variability30% 1/hét, de 1/nap 2/hó provokál I. Epizodic Havonta többször, de nem minden héten 1 hét, a rohamok között tünetmentesség PEF normál 2/hó Hosszabb futás köhögést és bronchospazmust provokál FEV1 80% PEF variability20% Treatment 1. 1. Controllers (Anti-inflammatory) *ICS, inhaled corticosteroid: (budenosid, fluticasone, beclomethason, ciclesonide) *oral or intravenous corticosteroids (prednisone, methylprednisolone, hydrocortisone) *leukotriene inhibitors (montelukast, zafirlukast, pranlukast) *LABA(long acting beta-2 agonists) – salmeterol, formoterol Treatment 2. 2. Releavers (bronchodilators ) *beta-2 agonist: - short-acting (SABA): inhaled (salbutamol, terbutalin, formoterol) *aminophylline or theophylline (I.v) *anticholinergics (ipratropium) GINA 2009 : treatment decrease 1. step 2. step increase 3. step p.r.n. SABA 5. step p.r.n. SABA Choose one ICS low dose antileukotriens Preventive treatment 4. step Choose one Copmbine one or more ICS low dose + LABA ICS moderate or high dose + LABA ICS moderate or high dose antileukotriens ICS low dose + antileukotrien ICS low dose + theophyllin, antileukotrien theophyllin Combine one or more oral corticosteroid (small dose) Anti IgE Severity of asthma exacerbations I. dyspnea Talks in Mild Moderate Severe Walking Can lie down sentences Talking Prefers sitting phrases At rest Hunched forward words Usually agitated Usually agiteted Increased >30/min alertness Respirator y rate Increased Resp.arrest Drowsy or confused Severity of asthma exacerbations II. Mild Moderate Severe Resp.arrest Accesory muscles not usually usually wheeze moderate loud Usually loud Paradox thoracoabdominal movement Abscence of wheeze Pulse rate <100 100-120 >120 Pulsus Absent 10-25 paradoxus <10mmHg mmHg bradycardi a >25mmHg Abscence musc.fatig. Severity of asthma exacerbations III. PEF Mild Moderate Severe >80% 60-80% <60% PaO2 >60mmHg <60mmHg PaCO2 <45mmHg >45mmHg SaO2 >95% 91-95% <90% Resp.arrest Treatment of acute exacerbation