Pharmacy Practice Innovations
advertisement

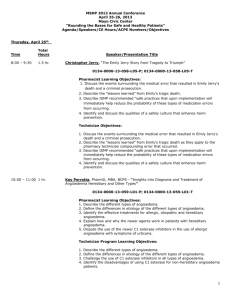
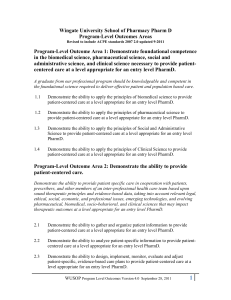
Pharmacy Practice Innovations: Best Practices in Care Transitions Michelle Cudnik, PharmD John Moorman, PharmD, BCPS June 27th, 2013 Michelle Cudnik, PharmD Clinical Ambulatory Care Lead Pharmacist, Summa Health System Associate Professor of Pharmacy Practice, NEOMED Local Ohioans Uninsured The percentage of persons aged 18 to 64 without health insurance Source: Powel, C “Health care issue stirs emotion because it is so personal”, Akron Beacon Journal, 7 October 2012, Available at http://www.ohio.com/news/local/health-care-issue-stirs-emotion-because-it-is-so-personal-1.340025 © 2012 What is the highest percentage of admission rates seen in the country that are due to 30-day readmissions? 1. 2. 3. 4. 15% 17% 19% 21% Hospital Readmissions Medicare 30 day readmissions as a percentage of admissions in 2009 Source: “Improving Care Transitions,” Health Affairs, September 13, 2012, Available at http://www.healthaffairs.org/healthpolicybriefs/ © 2012 Why a new model? • Institute of Medicine Report 2001, “Crossing the Quality Chasm” – Less than 50% of patients with major chronic illness receive accepted treatments – Less than 50% have satisfactory disease control – Focus on episodic and not continuous care – Little attention given to the patient’s knowledge, skills, behavior in managing their own illness Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington DC. National Academy Press; 2001 A tested Model: PCMH • • • • • Patient-centered (using patient goals) Physician-guided (EBM, directs the team) Cost-efficient Reimbursable (sustainable) Longitudinal, (goals persist through many contacts over time) • A continuous healing relationship (not just services) • Care provided in a variety of settings-Transitions are Key! • “Medical Home” refers to primary responsibility to assemble and interpret data and assist patient with self care of disease The Advanced Medical Home. American College of Physicians Policy Monograph, 2006 • National and Regional Relevance • • • • Model is centerpiece of Affordable Care Act, 2009 Meaningful Use (15 required core objectives; 5 menu objectives) Accountable Care Organization: (89 nationally under Center for Medicare and Medicaid services) NCQA (National Committee for Quality Assurance) Patient Centered Medical Home certification They all require: •A new practice focus on quality outcomes. •Exchange level data systems to track and report outcomes. •Care delivery systems require team-based care to achieve outcomes. www.cms.gov for meaningful use www.innovation.cms.gov for accountable care organizations 2011 Patient-Centered Medical Home Standards • • • • • • Enhance Access and Continuity Identify and Manage Patient Populations Plan and Manage Care Provide Self-care and Community Support Track and Coordinate Care Measure and Improve Performance National Committee for Quality Assurance 2011 System Multiple care Settings/Pharmacy Sub-specialist clinicians and services EHR Health Information Exchange Mid level provider NP/PharmD Office Administrator , Greeter Care coordinator RN/LPN/M A Care Plan Patient Centered Home Roles Patient Portal Family member, caregiver PCP Patient Office Patient and family System Multiple care Settings/Pharmacy Sub-specialist clinicians and services EHR Health Information Exchange Office Administrator , Greeter Care coordinator RN/LPN/M A Identifies, follows high risk patients • Assembles PreVisit results • Follows up on care plan Patient Centered Home Roles • Mid level provider NP/PharmD Patient Portal Family member, caregiver PCP Patient Office Patient and family Summa Health System • 8 hospitals and centers representing over 2,000 inpatient beds • Summit County’s largest employer with over 10,000 employees • 1,200 credentialed physicians and 280 resident physicians • One of top 3 largest integrated healthcare delivery systems in Ohio • Health Plan (SummaCare) • Affiliated with NEOMED University Summa Health System Payer Mix • • • • Commercial/Managed Care: 30% Self-Pay: 7% (27% in Internal Medicine Center) Medicaid: 15% Medicare: 47% My Practice • Akron City Hospital- Internal Medicine Clinic • Shared Faculty with NEOMED • 12,000 patients (mostly indigent) • Certified PatientCentered Medical Home A Day in the Life… • • • • Collaborative Practice Agreement Daily Huddles- identify high-risk patients Diabetic Planned visits 3 days per week Hypertension Clinic visits 1 day per week • Medication Therapy Management visits each day A Day in the Life… • Key member of the Patient-centered medical home! • Plan and manage care, coordinate follow-up visits, interface with community pharmacies and focus on continuity of care. • Facility fee billing Successes • Continued improvement in clinical outcome measurements in our diabetic patients • Improved education to medication residents, faculty and staff in the Internal medicine center • Comprehensive medication reconciliation completed at all visits Barriers • Initial delay in collaborative practice agreement • Knowledge by healthcare providers of what a pharmacist can offer to patients • Financial reimbursement for services Next Steps • Pilot study of a pharmacist in various primary care clinics within our healthcare system- different days of week (Resources by ACO?) • Focus on transitions of care for highestrisk patients • Reimbursement for Transitions of Care visits John Moorman, PharmD, BCPS Pharmacotherapy Specialist, Endocrinology, Akron General Medical Center Assistant Professor of Pharmacy Practice, NEOMED “The scenario in which a patient moves from one care setting to another” Cost of poor care transition 34,500 patients discharged and readmitted on the same day in 1996-1997 Cost = $226 million J. Gibbs Brown, personal communication, February 11, 2000 Cost of poor care transition 20% of Medicare hospitalizations followed by readmission within 30 days in 2003-2004 ~50% had no physician visit before readmission N Engl J Med 2009;360:1418-28 Cost of poor care transition 19% of Medicare discharges followed by adverse event within 30 days 66% were drug-related Ann Intern Med 2003;138:161-7 Cost of poor care transition Potential for cost savings by preventing unplanned readmissions $17.4 billion N Engl J Med 2009;360:1418-28 Cost of poor care transition A decrease in diabetes medication adherence results in a 58% increase in hospitalizations …and an 81% increase in all-cause mortality Arch Intern Med 2006;166:1836-41 National Transitions of Care Coalition (NTOCC) • Implementation and evaluation outline • Multiple resources developed: – TOC checklist – Interventions for low health literacy – Standardized forms – Metrics for tracking outcomes General recommendations • • • • • • • Improve communication Implement electronic medical records Establish points of accountability Increase use of case management Expand role of pharmacist in TOC Implement payment systems Develop performance measures When implementing a new TOC service, when should one decide which metrics to track? 1. Once management has been approached 2. Once personnel have been hired 3. Once a gap in care has been identified 4. Once a service has been implemented Akron General Medical Center • 511 adult-bed teaching hospital – Affiliated with Northeast Ohio Medical University • Significant proportion of admissions for underserved patients Personal experiences with TOC A day in the life… • Inpatient diabetes management team – Endocrinologist – Pharmacist – Diabetes educators (RN, CDE) – Dieticians • Outpatient transitional care clinic – “Bridge” clinic – Private endocrinology practice Interventions • • • • Inpatient education Medication reconciliation Involve social work/care management Plan development – Medication regimen – Goals of therapy – Follow-up Follow-up structure • Follow-up plan established – Discharge location – Need for transitional care visit? • “Bridge” clinic appointments set as inpatient – Not intended as chronic management – Communicated to primary care physician “Bridge” clinic • • • • Review of discharge medication list Goals of therapy reviewed Education/Literature provided Medication therapy performed if needed – Collaborative practice agreement • Follow-up plan established • All information sent to primary care Successes • Initially, patients instructed to call for appointment – Scheduling while inpatient improved show rate • As “Bridge” appointments increased, readmission rates decreased – Significantly lower than general readmission rate • Increased consultations by hospitalist groups/attending physicians Barriers • Private practice vs. health system – Inability to bill for services – Use of EMR limited • Limited to patients seen on inpatient service – Collaborative practice agreement – Concern over number of consults per physician • Length of stay Next steps • Diabetes Needs Assessment – Diabetic patients admitted to hospital prompts immediate referral – Triage based on need for education/management • Increase exposure to at-risk population • Intention to begin education on day 1 – Potential for decreased length of stay • Avoids “last-hour” consultations – Identify barriers earlier in hospital stay Conclusions • Established role for pharmacists in TOC – Diabetes vs. other disease states – Role needs to be expanded • Multiple interventions shown to be beneficial – Discharge counseling/med rec. • Implementing programs may be challenging – Requires focused approach with proper personnel – Know metrics before implementing Conclusions • These are just 2 models that focus on pharmacists involvement in transitions of care/continuity of care • These models can be adapted to other settings to provide innovative pharmacy services! Thank you for your attention! Questions?