Azacitidine in AML/MDS after allogeneic HSCT
advertisement

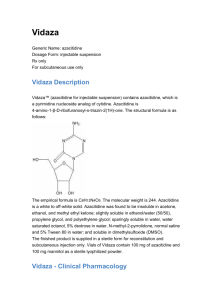
台北榮總血液腫瘤科 楊元豪/高志平大夫 Background Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the only potentially curative treatment in patients with advanced myelodysplastic syndromes (MDS) or acute myeloid leukemia (AML) Treatment for disease relapse after allo-HSCT is limited to conventional salvage chemotherapy, second allo-HSCT and donor lymphocyte infusion (DLI) DLI induce sustained second remission in some patients but also severe graft-versus-host disease (GVHD) 2 Azacitidine CALGB 9221 A randomized controlled phase III trial of subcutaneous azacitidine in MDS Patients: AML with marrow blasts 20-30% under current WHO criteria Treatment: subcutaneous 75 mg/m2/d x7 days q28d x4 courses v.s. best supportive care (BSC) Azacitidine improved response rate and time to leukemia transformation in MDS but not overall survival (OS) -Silverman LR, et al., JCO 2002 3 CALGB 9221: Azacitidine v.s. BSC Time to leukemia transformation P=0.007 OS P=0.10 4 Azacitidine Fenaux P, JCO 2010 Phase III randomized trial Patients: elderly patients (median age 70 y) with AML with marrow blasts 20-30% under current WHO criteria Treatment: subcutaneous azacitidine 75 mg/m2/d v.s. BSC only, low-dose cytarabine, or intensive chemotherapy Azacitidine significantly prolongs OS compared with conventional care regimens (CCR) 5 Azacitidine v.s. CCR OS P=0.005 6 Azazitidine after failed allo-HSCT Bolaños-Meade J, BBMT 2011 Retrospective study Between 2007 and 2009 at Johns Hopkins Hospital Patients: 10 patients with myeloid malignancies that received 5-azacytidine after a failed allo-HSCT Treatment: mostly 75 mg/m2/day for either 5 or 7 days 7 Outcomes of the patients 8 Discussions In the study cohort, azacitidine results in sustained responses in many of the patients without exacerbation of GVHD Hypomethylating agents including azacitidine may reverse the loss of tumor antigens and enhance graftversus-tumor reactions 9 RELAZA trial An open-label, single-center phase II trial Patients: CD34+ MDS or AML after allo-HSCT Treatment: azacitidine in the setting of minimal residual disease (MRD)-triggered pre-emptive therapy Purpose: to prevent or delay hematologic relapse in patients -Platzbecker U, et al., Leukemia 2012 10 CD34+ donor chimerism CD34+ donor chimerism analysis: <80% in the peripheral blood predicts almost unavoidable relapse in all patients, even in the presence of intervention of immediate interruption of immunosuppression or DLI in a median of 61 days 11 Patients Inclusion Aged >18 years CD34+ MDS or AML After allo-HSCT CD34+ for leukemic blasts Exclusion Hematologic relapse Severe hepatic impairment Severe renal impairment 12 Patients Screening CD34+ donor chimerism in the PB Monitored 3-4 weeks during the first 8 months, and 7-8 weeks during months 8-24 Patients who experienced a drop in CD34+ donor chimerism below 80% without concurrent hematologic relapse (<5% bone marrow blats) entered the treatment phase 13 Methods Treatment 4 cycles of azacitidine 75 mg/m2/day subcutaneously on days 1-7 Repeated cycle on day 29+/-2 Major response: increase of CD34+ donor chimerism in PB >80% Minor response: increase of CD34+ donor chimerism in PB but <80% Additional 4 cycles in patients with minor response and stabilization or further decrease of CD34+ donor chimerisim 14 Methods Dose adjustment No adjustment: WBC >3x10^9/L, Plt >50x10^9/L 67% in WBC 1-3x10^9/L, Plt 25-50x10^9/L DC in WBC <1x10^9/L, Plt <25x10^9/L Immunosupressions Could be withdrawn to support relapse prevention Antibiotics Antibiotic prophylaxis is permitted 15 Results A total of 59 patients entered the screening phase A total of 20 patients experienced a drop of CD34+ donor chimerisim <80% and enrolled into the treatment phase 16 17 18 Summary of clinical responses 19 20 21 22 23 24 Disease course of a patient with repeated major response 25 Results 13 patients (65%) in the intent-to-treat population had relapsed within a median of 231 days after first MRD detection 8 patients (40%) were alive with a median follow-up of 487 days after the first detection of MRD There was no GVHD reported in patients without a prior history of GVHD Complete cessation of immunosuppressive treatment was possible in 4 of 6 patients without exacerbation of GVHD, even with history of GVHD 26 Discussions After only 4 cycles of azacitidine, MRD was diminished or stabilized in 80% of patients Response were continuous without any further treatment in 4 of these patients But, for the majority, hematologic relapse finally occurred in 13 patients at a median of 231 days 27 Discussions Studies in mice suggest azacitidine induced FOXP3 expression in naïve T-cells, which in turn induces a regulatory T-cell population that mitigate GVHD while preserving a GVL effect 28 Conclusions MRD-triggerd treatment with azacitidine is an effective strategy to prevent or to delay hematologic relapse in patients with MDS or AML after HSCT. Azacitidine may enhance GVL reaction and, conversely, may prevent GVHD. The development of larger, prospective trials to evaluate the efficacy of azacitidine after allo-HSCT is necessary. 29