liver cirrhosis-2
advertisement
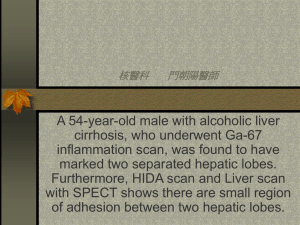
LIVER CIRRHOSIS DEFINITION: pathological condition with the development of fibrosis to the point that there is architectural distorsion with formation of regenerative nodules CAUSES: • Alcoholism • Chronic viral hepatitis (Hepatitis B, Hepatitis C) • Autoimmune hepatitis • Nonalcoholic steatohepatitis • Billiary cirrhosis • Primary billiary cirrhosis • Primary sclerosing cholangitis • Autoimmune cholangiopathy • • • • • • • Cardiac cirrhosis Metabolic liver disease: Hemocromatosis Wilson’s disease L1 Antitrypsin deficiency Cystic fibrosis Cryptogenic cirrhosis ALCOHOLIC CIRRHOSIS •14 milion adults in US -alcohol abuse or dependence •10th most common cause of death in adults • alcoholic cirrhosis accounts 40% of deaths due to cirrhosis CLINICAL FEATURES • • • • • • • • • • • • NON SPECIFIC SYMPTOMS: vague right upper quadrant pain fever nausea and vomiting diarrhea anorexia malaise LATER , SPECIFIC COMPLICATIONS: ascites edema bleeding (UDH) jaundice/encephalopathy • incidentally at the time of autopsy or elective surgery PHYSICAL EXAMINATION • liver and spleen enlarged with the liver edge firm and nodular • scleral icterus • palmar erythema • spider angiomas • parothid gland enlargement • digital clubbing • muscle wasting • edema and ascites • decreased body hair, gynecomastia • testicular atrophy • menstrual irregularities/ amenorrheic women These changes are often reversible following cessation of alcohol - LABORATORY TESTS DIAGNOSIS normal in patients with early compensated alcoholic cirrhosis • Clinical features + physical examination findings + laboratory studies • Liver biopsy,ultrasonography, UDE,CT ( dg. dif. Cancer) (abstinence maintained 6 months-> residual, nonreversible disease) - in advanced liver disease many abnormalities are present: • anemia (chronic GI blood lose, nutritional deficiencies, hipersplenism related to portal hypertension , hemolytic anemia- ZIEVE’S syndrome) • platelets counts are often reduced early (PHT) • total direct bilirubin- N/ elevated • protrombin times prolonged • AST>ALT2:1ratio Patients who have had complications and who continue to drink have a <50% 5-year survival in contrast with those who remain abstinent ->prognosis improved and LIVER TRANSPLANTATION - VIABLE OPTION TREATMENT • • • • Abstinence- cornerstone therapy Good nutrition and long term medical supervision Glucocorticoids are occasionally used(DF>32) Oral PENTOXIFYLINE decrease tumour necrosis factor alpha (TNF-alpha) and other proinflamatory cytokines • Parenterally adm. of inhibitors of TNF-alpha (INFLIXIMAB/ ETANERCEPT) • Medication that reduce craving for alcohol ACAMPROSATE CALCIUM • Vit.B1,B6,B12+SG10%,Arginine,Aminohepa,Aspat ofort CIRRHOSIS DUE TO CHRONIC VIRAL HEPATITIS B OR C • patients exposed to the hepatitis C (HCV) - 80% develop chronic hepatitis C and ,of those,-20-30% will develop cirrhosis over 20-30 years •world wide , 170 million individuals have hepatitis C •progression of liver disease due to chronic HC is characterized by : •portal- based fibrosis with brindging fibrosis and nodularity developing --> cirrhosis •inflammatory infiltrate in portal areas •lobular hepato-cellular injury and inflammation •HCV genotype 3, steatosis is often present •Hepatitis B exposure : 5% develop chronic hepatitis B, 20% will go to develop cirrhosis •in US 1,25 million carriers of HB; Asia, Africa 15%aquires the infection vertically (at birth) and 25% may develop cirrhosis CLINICAL FEATURES • fatigue • malaise • right upper quadrant pain LABORATORY EVALUATION • HCV-RNA,genotype • AgHBS • anti HBS • HBe Ag • anti HBe • HBV-DNA levels TREATMENT IN HEPATITIS B • • • • LAMIVUDINE100mg/day ADEFOVIR ENTECAVIR 0.5mg/day TENOFOVIR INTERFERON ALFA should not be used in decompensated cirrhotics with EV,ascites,jaundice CIRRHOSIS FROM AUTOIMMUNE HEPATITIS •Positive autoimmune markers ANA,ASMA •Active inflammation - elevated liver enzimes->immunosuppresive therapy •Obesity in western countries - patients with nonalcoholic fatty liver disease •Management of complications of cirrhosis due to AIH or NASH is similar to that for other forms of cirrhosis BILLIARY CIRRHOSIS Cholestatic liver disease result from necroinflammatory lesions : •congenital •metabolic processes •external bile duct compresion 2 broad categories reflect the anatomic sites of abnormal bile retention : •intrahepatic -- different approach •extrahepatic--surgical/endoscopic biliary tract decompression PBC (primary biliary cirrhosis) 100-200 / million(female preponderence / median age - 50 years )-at the time of diagnosis Cause: unknown It is characterized by portal inflammation and necrosis of cholangiocytes in small and medium size bile ducts Lab findings: elevated bilirubine level progressive liver failure LIVER TRANSPLANTATION- treatment of choice for patients with decompensated cirrhosis URSODEOXYCHOLIC ACID (UDCA) AMA - 90% patients with PBC - useful markers for PBC PBC (primary biliary cirrhosis) CLINICAL FEATURES LABORATORY FINDINGS : • • • fatigue pruritus 50% - bothersome in the evening; prior to jaundice (severe disease and poor prognosis) • • • PHYSICAL EXAMINATION • JAUNDICE • hepatomegaly • splenomegaly • ascites • edema • hiperpigmentation-trunk,arms • xantelasma (xanthomata) • bonepain : osteopenia/osteoporosis • scratching lesions augmentation of GGT, ALP, ALT, AST, IgM hiperbilirubinemia trmobocytopenia , leucopenia, anemia -- PHT, hipersplenism LIVER BIOPSY - 10% AIH, “overlap” syndrome DIAGNOSIS Patients with chronic colestatic liver enzyme abnormalities in middleaged women AMA +/- (10%) --> biopsy TREATMENT • UDCA (early initiated 13-15 mg/kg/day) improve bichemical and histological features; it does not reverse and cure the disease; side effects: diarrhea, headache • LIVER TRANSPLANTATION –decompensated disease • Antihistamines • Narcotic receptor antagonist (naltrexone) • Rifampin • Cholestyramine-bile salt sequestering agent • Plasmapheresis intractable pruritus • Bisphosphonate should be instituted when bone disease is identified (bone density testing) PRIMARY SCLEROSING CHOLANGITIS Definition: chronic cholestatic syndrome – diffuse inflamation, fibrosis involving the entire biliary treeobliteration of both intra and extrahepatic biliary tree, leading to biliary cirrhosis / portal hipertension/ liver failure Cause: unknown •bile duct proliferation, ductopenia, pericholangitis •liver biopsy : periductal fibrosis PRIMARY SCLEROSING CHOLANGITIS CLINICAL FEATURES : • fatigue profound and nonspecific • pruritus • steatorrhea • deficiencies of fat – soluble vitamins • metabolic bone disease LABORATORY FINDINGS: • abnormal liver enzymes (>2 ALP and ↑ AST,ALT) • albumin levels ↓ • TP↑ • overlap syndrome between PSC and AIH • autoantibodies + in overlap syndrome , - in PSC alone (only); P-ANCA is + in 65% of those with PSC; in PSC50% patients have UCcolonoscopy PRIMARY SCLEROSING CHOLANGITIS DIAGNOSIS • colangiographic imaging-multifocal stricturing and beading • MRCP-initial evaluation • ERCP-whether or not a dominant stricture is present The strictures are typically short with intervening segments of normal or slightly dilated bile ducts diffusely distributed beaded appearance Gallbladder, cystic duct involved in 15% of cases;evolution gradually to biliary cirrhosis decompensation with ascites , esophageal variceal hemorrhage , encephalopathy TREATMENT • • • • nonspecific high-dose (20mg/kg/day) UDCA endoscopic dilatation of strictures LIVER TRASPLANTATION (LT) ; Cholangiocarcinoma relative CI for LT HEMOCHROMATOSIS DEFINITION: inherited disorder of iron metabolism that results in a progressive increase in hepatic iron deposition whitch , over time, can lead to a portal-based fibrosis progressing to cirrhosis / liver failure/ hepatocellular cancer Serum iron studies : • elevated transferin saturation • ↑ feritine level • HFE mutation analysis TREATMENT is straight forward with regular therapeutic phlebotomy WILSON’S DISEASE DEFINITION: inherited disorder of cooper homeostasis with failure to excrete excess amounts of cooper , leading to accumulation in the liver. 1/30000 individuals; affects adolescents and young adults DIAGNOSIS: • ceruloplasmin levels • 24-hours urine cooper levels • liver biopsy PHYSICAL EXAMINATION - KAYSER-FLEICHER corneal ring TREATMENT : cooper chelating medication (DPENICILLAMINE/TRIENTINE/Zn) ALFA1-AT DEFICIENCY DEFINITION: inherited disorder that causes abnormal folding of the alfa-1AT PROTEIN->failure of secretion of that protein from the liver 22 genotype / 10-20% - chronic liver disease DIAGNOSIS: • determining of alfa1 AT levels/ genotype • liver biopsy : PAS+ ; diastase- resistant globules TREATMENT: LT is curative COMPLICATIONS OF CIRRHOSIS • Portal hypertension: -GE varices -portal hypertensive gastropathy -splenomegaly, hypersplenism -ascites -SBP • Hepatorenal syndrome I,II • Hepatic encephalopaty • Hepatopulmonary syndrome • Portopulmonary hypertension • Malnutrition • Bone disease: -osteopenia -osteoporosis -osteomalacia • Hematologic abnorm.: -anemia -hemolysis -neutropenia -trombocytopenia - coagulopathy TREATMENT FOR VARICEAL HEMORRHAGE : 1. PRIMARY PROPHYLAXIS 2. PREVENTION OF RECURRENT BLEEDING 1. PRIMARY PROPHYLAXIS - screening by endoscopy of all patients with cirrhosis -non-selective betabloblokers or variceal band ligation / sclerotherapy ((PROPRANOLOL, NADOLOL) -hepatic vein pressure >12 mmHg ACUTE BLEEDING : • • • • • fluid and blood product replacement prevention of subsequent bleeding with EVL vasoconstrictive agenta : SOMATOSTATIN , OCTREOTIDE 50-100 ug/h by continuous infusion (VASOPRESIN -in the past) BALLON TAMPONADE (Sengstaken-Blakemore tube / Minnesota tube)--> stabilisation prior to endoscopic therapy esophageal varices extended into the proximal stomach - TRANSJUGULAR INTRAHEPATIC PORTOSYSTEMIC SHUNT (angiographic guidance) 2. PREVENTION OF RECURRENT BLEEDING • repeated VBL until varices are obliterated • betablockade- recurrent VBL • portosystemic shunt surgery , TIPS for patients with good hepatic synthetic function who could benefit by having portal decompressive surgery. MANAGEMENT OF RECURRENT VARICEAL HEMORRHAGE RECURENT ACUTE BLEEDING ENDOSCOPIC THERAPY +/- PHARMACOLOGIC THERAPY CONTROL OF BLEEDING ↓ COMPENSATED CIRRHOSIS (CHILD’S CLASS A) ↓ SURGICAL SHUNT VS. TIPS ↓ LIVER TRANSPLANTATION ↓ DECOMPENSATED CIRRHOSIS ( CHILD’S CLASS B,C) ↓ TRANSPLANT EVALUATION ↓ ENDOSCOPIC THERAPY OR BETABLOKERS ↓ TIPS ↓ LIVER TRANSPLANTATION ASCITES TREATMENT • 1.Dietary sodium restriction-small amounts of ascites 6-8g/day ,<2g/day in>ascites • Fresh, frozen foods • 2.Diuretic therapy-moderate amounts of ascites:Spironolactone100-200mg/day,4600mg/day+Furosemide40-80mg/day(peripheral edema);120-160mg/day-necompliant patients. • 3.Repeated large volume paracentesis,TIPS,liver transplantation(<50% survive 2years after the onset of ascites). HEPATIC ENCEPHALOPATHY • Ammonia levels>,mercaptans • 1.Hydration and correction of electrolyte imbalance • 2.Replacing animal-based protein with vegetable-based protein • 3.Lactulose-elimination of nitrogenous products(2-3soft stools/day) • 4. Nonabsorbed antibiotics:Neomicine/Metronidazole(renal failure,ototoxicity,peripheral neuropathy),RIFAXIMINENORMIX,NO side effects. • 5. ZN supplementation SPONTANEOUS BACTERIAL PERITONITIS • Neutrophil count>250/mm3 • Occur in 30%of patients with SBP and25% in hospital mortality rate • Escherichiacoli/gram+bacteria(Streptococcus viridans,Staphilococcus aureus,Enterococcus • Second –generation cephalosporin-CEFOTAXIM 4g/day • In those with UDB,the frecquency of SBP is increased and prophylaxis against it is recommended HEPATO-RENAL SYNDROME • Functional renal failure without renal pathology that occurs in 10% of patients with advanced cirrhosis or acute liver failure • Step-wise progressive increase in creatinine in those with large amount of ascites • TYPE 1 HRS:progressive impairment in renal function and >reduction in creatinine clearance within 1-2 weeks of presentation • TYPE 2 HRS: reduction in glomerular filtration rate with >serum creatinine level(better outcome than type 1 HRS!) • Dopamine,PG analogs • Midodrine(alpha-agonist) • Octreotide • Albumine i.v. • LIVER TRANSPLANTATION