Kidneys Excrete Excess Water (cont.)
advertisement

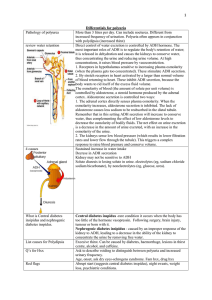
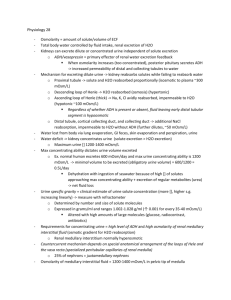
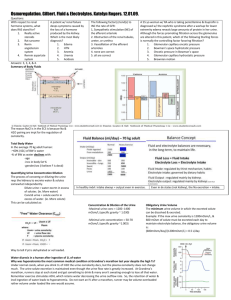
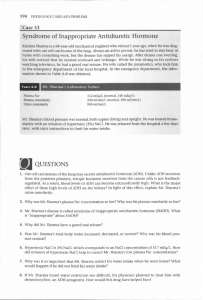
Chapter 28: Urine Concentration and Dilution; Regulation of ECF Osmolarity and Sodium Concentration Guyton and Hall, Textbook of Medical Physiology, 12th edition Kidneys Excrete Excess Water by Forming Dilute Urine • ADH (Vasopressin) Controls Urine Concentration • Renal Mechanisms for Excreting Dilute Urine Fig. 28.1 Water diuresis in a human after ingestion of 1 liter of water Kidneys Excrete Excess Water by Forming Dilute Urine Fig. 28.2 Formation of dilute urine when ADH levels are very low Kidneys Excrete Excess Water (cont.) a. Tubular fluid remains isosmotic in the proximal tubule b. Tubular fluid is diluted in the ascending loop of Henle c. Tubular fluid in the distal and collecting tubules is further diluted in the absence of ADH Kidneys Conserve Water by Excreting Concentrated Urine • Water Deficit—kidney excretes solutes but reabsorbs water therefore decreasing the volume formed • Urine Specific Gravity Fig. 28.3 Relationship between specific gravity and osmolarity of the urine Kidneys Conserve Water by Excreting Concentrated Urine • Requirements for Excreting a Concentrated Urine a. High levels of ADH b. High osmolarity of the renal medullary interstitial fluid Kidneys Conserve Water by Excreting Concentrated Urine • Countercurrent Mechanism Produces a Hyperosmotic Renal Medullary Interstitium a. Buildup of solute concentration in the medulla 1. Active transport of Na and cotransport of K, Cl, and other ions from the loop of Henle 2. Active transport of ions from the collecting ducts 3. Facilitated diffusion of urea from collecting ducts 4. Diffusion of water from the tubules Table 28.1 Summary of tubule characteristics—urine concentration Active NaCl Transport Water Permeability NaCl Permeability Urea Permeability Prox. Tubule ++ ++ + + Thin descending 0 ++ + + Thin Ascending 0 0 + + Thick Ascending ++ 0 0 0 Dist. Tubule + +ADH 0 0 Cortical Coll. Tubule + +ADH 0 0 Inner med. Coll. Duct + +ADH 0 ++ADH Conserving Water (cont.) • Steps Involved in Causing Hyperosmotic Renal Medullary Interstitium Fig. 28.4 Countercurrent multiplier system in the loop of Henle for producing a hyperosmotic renal medulla (values are in milliosmoles per liter Conserving Water (cont.) • Role of Distal Tubule and Collecting Ducts in Excreting Concentrated Urine Fig. 28.5 Formation of a concentrated urine when ADH levels are high. Conserving Water (cont.) • Urea Contributes to Hyperosmotic Renal Medullary Interstitium and Formation of Concentrated Urine • Recirculation of Urea from Collecting Duct to Loop of Henle Contributes to Hyperosmotic Renal Medulla a. In general the rate of urea excretion is determined by 1. The concentration of urea in the plasma 2. The glomerular filtration rate Fig. 28.6 Recirculation of urea absorbed from the medullary collecting duct into the interstitial fluid Conserving Water (cont.) • Countercurrent Exchange in the Vasa Recta Preserves Hyperosmolarity of the Renal Medulla a. Two features that contribute to the preservation of high solute concentrations 1. The medullary blood flow is low 2. The vasa recta serve as countercurrent exchangers • Increased Medullary Blood Flow reduces Urine Concentrating Ability Fig. 28.7 Countercurrent exchange in the vasa recta Conserving Water (cont.) • Summary of Urine concentrating Mechanism and Changes in Osmolarity in Different Segments of the Tubules Fig. 28.8 Control of ECF Osmolarity and Sodium Concentration • Estimating Plasma Osmolarity from Plasma Sodium Concentration a. Na ions in the ECF and associated anions are the principal determinants of fluid movement across the cell membrane Osmoreceptor-ADH Feedback System Fig. 28.9 Osmoreceptor-ADH feedback mechanism for regulating ECF osmolarity in response to a water deficit Osmoreceptor-ADH Feedback System • ADH Synthesis in the Hypothalamus and Release from the Posterior Pituitary Fig. 28.10 Osmoreceptor-ADH Feedback System • Stimulation of ADH Release a. Arterial baroreceptor reflexes b. Cardiopulmonary reflexes c. Decreased arterial pressure d. Decreased blood volume Osmoreceptor-ADH Feedback System • Either a decrease in effective blood volume or an increase in ECF osmolarity stimulates ADH secretion Fig. 28.11 The effect of increased plasma osmolarity or decreased blood volume on the level of plasma ADH Importance of Thirst in Controlling ECF Osmolarity and Na Concentration Table 28.2 Regulation of ADH Secretion Increase ADH Decrease ADH plasma osmolarity plasma osmolarity blood volume blood volume blood pressure blood pressure Nausea Nausea Hypoxia Hypoxia Drugs: Drugs: Morphine Alcohol Nicotine Clonidine (antihypertensive) Cyclophosphamide Haloperidol (dopamine blocker) Thirst (cont.) • Stimuli for Thirst a. Increased ECF osmolarity which causes intracellular dehydration in the thirst centers b. Decrease in ECF volume and arterial pressure c. Production of angiotensin II d. Dryness of the mouth and mucous membranes e. GI and pharyngeal stimuli • Threshold for Drinking – when the Na concentration increases 2 mEq/L above normal, the thirst mechanism is activated