Congenital Myasthenic Syndromes (CMS)
advertisement

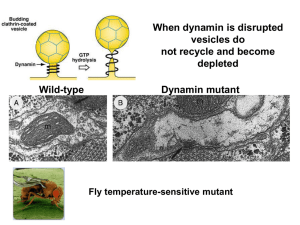
Congenital Myasthenic Syndromes Shahriar Nafissi, MD Associate Professor of Neurology Tehran University of Medical Sciences Physiology The Neuromuscular Junction Action Presynaptic potential channel terminal Ca2+ Ca2+ action potential opening voltage-gated Ca2+ channels ↑Ca2+ permeability Ca2+ Presynaptic Ca2+ terminal channel ACh ↑Ca2+ Ach release from synaptic vesicles Synaptic cleft Na+ ACh Na+ Receptor molecule ACh binding to Ach receptors opening ligand-gated Na+ channels. Na+ Action potential Na+ Action potential ↑Na+ permeability depolarization action potential generation in the postsynaptic membrane ACh Choline Acetic acid ACh receptor site Acetylcholinesterase Ach →acetic acid + choline ▲ Ach-Esterase Presynaptic terminal ACh Acetic acid Synaptic vesicle Choline ACh Choline in the presynaptic terminal Choline + acetic acid → Ach → Synaptic vesicles Structural Reality By John Heuser and Louise Evans University of California, San Francisco Ligand- Gated Ion Channel 2α + β + ε + δ Congenital Myasthenic Syndromes • Group of diseases caused by genetic defects affecting neuromuscular transmission • Heterogeneous inheritance and pathophysiology Classification • Presynaptic Defect – Choline Acetyl Transferase deficiency – Paucity of synaptic vesicles – Lambert-Eaton like CMS • Synaptic Defect – Endplate ACh Esterase deficiency • Postsynaptic Defects – – – – – – Kinetic abnormality of AChR AChR deficiency Rapsyn Dok-7 SCN4A MuSK • No identified Defect percentage of CMS subtypes in different centers Diagnostic Clues in CMS • Weakness/fatigability of limbs and oculobulbar muscles • Early onset (since neonatal period) • Positive family history • EDX findings (RNS, SFEMG) • Response to anti-cholinesterases • Absence of anti-AChR, MuSK , VGCC antibodies Diagnostic Difficulties • Diagnostic problems – – – – – – Late onset (in adult) No response to anticholinesterases No family history Episodic symptoms No ophthalmoplegia or cranial involvement Decrement may not be present in all muscles, or present only intermittently • Misdiagnosed as – congenital myopathy – Seronegative MG (late onset) – Metabolic myopathies R ABD POLL BR EVIS Ampl (mV) over Study 5.0 2.5 0.0 1 24 Yo, referred as congenital myopathy Responsive to Mestinon 2 3 4 Electrodiagnosis • Decrement after 2-3 HZ RNS – Absent in ChAT def., Na-Channel CMS, Some cases of Rapsyn • If negative, try higher frequencies • Try conditioning with 5 minutes 10HZ stimulation • Single-Fiber EMG Electrodiagnostic clues • Repetitive CMAP after single stimulus • Low amplitude CMAP with significant increment after high frequency RNS • Response to Tensilon test Presynaptic Syndromes Choline-Acetyl Transferase deficiency (ChAT def.) • ± neonatal hypotonia, gradually improve • Attacks of apnea, bulbar paralysis precipitated after infection, fever, excitement • No symptoms or mild-myasthenic symptoms between attacks • Reduced number of attacks with increasing age • Treatment: – AchE Inh. for myasthenic symptoms and prophylaxis – IM AchE Inh. Injection on crisis Synaptic Defect Endplate ACh Esterase deficiency AChEsterase Clinical Features • Myasthenic symptoms since birth or early childhood • delayed milestones • Weakness facial, axial, limb± ophthalmoplegia • Fatigable lordosis and scoliosis • Finger extensor weakness • Slow pupillary light response •11 yo, weak since infancy with ptosis, restricted EOM, sluggish pupillary reflex, lordosis •Worsening with Mestinon, some response to pseudoephedrine Decrement after 3 HZ RNS Repetitive CMAP after single stimuli Catalytic Subunits Collagen Tail Formed by triple-helical association of three collagen strands (ColQ) Therapy • AchE inhibitors ineffective • Increased muscarinic side effects • Some improve with ephedrine or pseudo-ephedrine 20 yo, Ptosis since infancy Delayed walking, Ophthalmoparesis generalized weakness No reponse to mestinon, 3,4-DAP, Quinidine, fluoxetine Improved with ephedrine Mutation found in ColQ L ABD DIG MIN (UL) 1.1 1.2 1.3 Ampl (mV) over Study 1.4 10 1.5 1.6 5 1.7 2 0 1.8 1.9 1 2 3 4 5 1 3 5 4 1.10 30ms 2mV 16 yo, Lordotic gait from beginning, WCB from 11 No ptosis or ophthalmoparesis proximal > distal Diagnosed as DMD AChRAb negative Worse with Mestinon R ABD POLL BREVIS 1.1 1.2 1.3 1.4 1.5 1.6 2 1.7 1.8 1.9 1 5 3 1.10 30ms 500µV 4 R ULNAR - ADM R MEDIAN - APB 2 2 1 3 5 4 Wrist 1 30ms 5mV 16mA 14-33% decrement 1 Wrist 1 30ms 1mV 20mA Repetitive CMAP 2 2 1 3 4 5 B.Elbow 2 30ms 5mV 16mA 1 3 El bow 2 30ms 1mV 20mA Post-Synaptic Syndromes Post-Synaptic Syndromes • Kinetic abnormalities of AChR – Slow-Channel Syndrome – Fast Channel Syndrome • Low-Expressor AChR Deficiency • Rapsyn Deficiency • Sodium-Channel Myasthenia • Dok-7 Synaptopathy Slow-Channel Syndrome • Autosomal Dominant • Selective weakness of cervical, scapular, finger ext., • Eye movements: spared or mildly affected • Early onset: gradually progressive • Late onset and mild • Fluctuating • Severely affected muscles become atrophic • EMG – Repetitive CMAP after single stimuli – Decrement only in weak muscles • Pathogenesis – Prolonged AChR opening ↑ cations and Ca++ Ca++ excess activation of protease, lipase, free radicals endplate myopathy – Depolarization block Family M. Slow channel G153S Intra familial variability for severity mild severe • Pathology: tubular aggregates • Genetics: mutation in AChR subunits • D.D.: •Polyneuropathy •Motor Neuron Disease •Radial palsy •Mitochondrial disease •Limb-Girdle MD •Myotonic Dystrophy •FSHD Therapy • AChE Inh. Ineffective or only temporary improvement • Probably accelerate progression by cationic overload • Long-lived open channel AChR blockers – Quinidine 200 mg × 3-4/d – Fluoxetine 80 mg/d Ach Receptor Deficiency ε/ Low-Expressor AChR mutations • Reduced AChR expression to < 15% • Mild to severe phenotype • Most cases mutation in ε-subunit of AchR fetal AchR harboring γsubunit is substituted • Mutations in both alleles of a non-ε subunit incompatible with life • Most respond well to AChE Inh ± DAP •18 yo, referred as MG for a consult before rhinoplasty •Has always been weak in physical activity and if doing so, fatigued very fast. •Fluctuating ptosis and diplopia. •Stable and non-progressive during these years and worse in the evening •Significant subjective and objective improvement with Mestinon • Myasthenic symptoms since infancy • Very good response to mestinon • Both have been misdiagnosed as myasthenia gravis and both thymectomised • Mutation in CHRNE ( ε-subunit of AchR) Rapsyn Tyrosine kinase function : AChR concentration and linkage to cytoskeleton Rapsyn Deficiency • Has a crucial role in concentrating AChR in post-synaptic membrane • Birth or neonatal ± Arthrogryposis • Sometimes juvenile-adult onset • Facial deformity: prognathism, malocclusion • Severe masticatory weakness • Ptosis without ophthalmoparesis • Cervical, truncal, limb usually spared • Stable and benign course • EMG – Decrement not present in all – Single-Fiber EMG • Partial to well response to AChE Inh • Addition of 3,4-DAP sometimes beneficial DOK7 Synaptopathy Dok-7 interacts with MuSK and is essential for postsynaptic specialization of the neuromuscular junction DOK7 Synaptopathy Clinical features • Difficulty in walking developing after normal motor milestones • Proximal muscles weakness > distal • Ptosis often present, EOM rarely involved • EMG always abnormal – decrement in amplitude and/or – jitter and blocking on single-fiber studies • No benefit from anticholinesterase, sometimes worsened • Responded to ephedrine Clinical clues pointing to a specific diagnosis Endplate AChE deficiency ● Repetitive CMAPs ● Refractoriness to cholinesterase inhibitors ● Delayed pupillary light reflexes Slow-channel CMS ● Repetitive CMAPs ● Selectively severe involvement of cervical and wrist and finger extensor muscles in most cases ● Dominant inheritance in most cases Clinical clues pointing …-2 Endplate choline acetyltransferase deficiency ● Recurrent apneic episodes ● No or variable myasthenic symptoms between acute episodes ● EMG decrement at 2-3 Hz can be absent at rest but appears after stimulation at 10 Hz for 5 min, then disappears slowly. Rapsyn deficiency ● Multiple congenital joint contractures ● Increased weakness and respiratory insufficiency precipitated by intercurrent infections ● EMG decrement can be mild or absent. Dok-7 myasthenia ● Proximal greater than distal limb weakness, ● mild ptosis, and normal ocular ductions in the majority ● May deteriorate on exposure to pyridostigmine Standard pharmacotherapy • ChAT deficiency: AChEI oral prophylaxis, parenteral use in crisis • Achesterase deficiency: avoid AChEI; try ephedrine • AChR deficiency: AChEI; 3,4-DAP also helps in 30–50% • Slow-channel CMS: quinidine or fluoxetine • Fast-channel CMS: AChEI and 3,4-DAP • Rapsyn deficiency: AChEI; some benefit further from 3,4-DAP • Limb-girdle myasthenia: AChEI; some benefit from ephedrine • Dok-7: ephedrine ?