What are county administrative DMC expenses?
advertisement
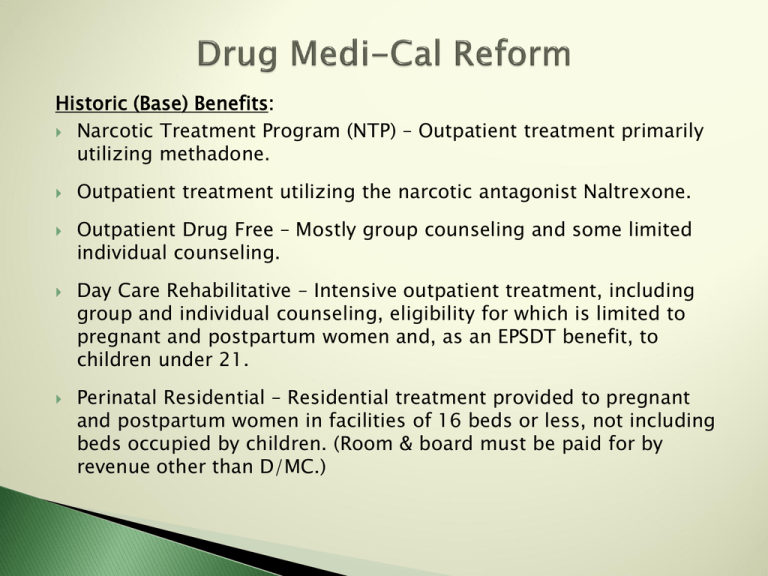
Historic (Base) Benefits: Narcotic Treatment Program (NTP) – Outpatient treatment primarily utilizing methadone. Outpatient treatment utilizing the narcotic antagonist Naltrexone. Outpatient Drug Free – Mostly group counseling and some limited individual counseling. Day Care Rehabilitative – Intensive outpatient treatment, including group and individual counseling, eligibility for which is limited to pregnant and postpartum women and, as an EPSDT benefit, to children under 21. Perinatal Residential – Residential treatment provided to pregnant and postpartum women in facilities of 16 beds or less, not including beds occupied by children. (Room & board must be paid for by revenue other than D/MC.) Enhanced DMC Benefits: Pursuant to new state statute (ABX 1 & SBX 1), the DMC benchmark benefits are based on the SUD benefits in the Kaiser Small Group Plan, and are now an entitlement for the Medicaid population. With the exception of residential treatment and detox, these enhanced benefits were added to the State Plan for Drug Medi-Cal. These enhanced benefits supplement, do not replace the current Drug Medi-Cal benefits. These benefits, like the historic DMC benefits, are available statewide. There is no county opt-in. The enhanced benefits are an entitlement for all Drug Medi-Cal eligible, not just for the newly-eligible (the expansion population). Enhanced Benefits (pursuant to ABX 1 & SBX 1): Intensive outpatient treatment programs for all DMC populations. Formerly called “daycare rehabilitative,” these services include outpatient counseling and rehabilitation services that are provided at least 3 hours per day, 3 days per week. Transitional residential recovery services for all DMC populations, including chemical dependency treatment in a nonmedical transitional residential recovery setting that provides counseling and support services in a structured environment, and inpatient voluntary detox in chemical dependency treatment facilities and freestanding psychiatric facilities. (Note: these benefits are not yet included in the DMC State Plan.) What is the current status of the residential treatment benefit? Although residential treatment for all DMC populations is one of the enhanced benefits in the state’s benchmark benefit plan, CMS has asked DHCS to remove this benefit from the State Plan because of the Institutions for Mental Disease (IMD) payment exclusion, a federal Medicaid rule that prohibits FFP for services provided to any individual between the ages of 21 and 65 who is a patient in an inpatient psychiatric or substance use disorder treatment facility with more than 16 beds. Currently, other than 11 perinatal residential programs, there are no residential SUD programs in California that receive Medicaid funding, due to the IMD exclusion. Consequently, only 1,825 beds of the total statewide 18,155 licensed beds for residential SUD treatment are reimbursable under Drug Medi-Cal. Other Medi-Cal SUD benefits that are not included in DMC: Medically necessary voluntary inpatient detoxification in general acute hospital settings; hospitalization for medical management of withdrawal symptoms, including room and board, physician services, drugs, dependency recovery services, education and counseling. (Note: this is provided as a Medi-Cal fee-for-service benefit.) Medication-Assisted Treatment – This service includes medications, other than methadone and naltrexone, that are used in the treatment of substance use disorders in outpatient settings. These medications are provided via Medi-Cal managed care of Medi-Cal FFS, depending on the medication. Screening and Brief Intervention – This service is available to the Medi-Cal adult population for alcohol misuse, and is provided in primary care settings via Medi-Cal managed care or FFS. DHCS is pursuing a DMC Organized Delivery System Waiver as an amendment to the current Section 1115 Bridge to Reform Demonstration Waiver. This amendment would demonstrate how organized SUD care increases successful outcomes for DMC beneficiaries. Key Program Elements of the Waiver: • • Continuum of Care: Participating counties will be required to provide a continuum of services, including early intervention, physician consultation, outpatient treatment, case management, medication-assisted treatment, recovery services, withdrawal management, and at least one level of residential treatment. * Assessment Tool: The ASAM assessment tool determines the most appropriate level of care, so that clients can enter the system at the appropriate level and step up or step down in intensity of services, based on their response to treatment. • • • • Case Management and Residency: Case management services will be required and funded to ensure that the client is moving through the continuum of care. Counties will be required to coordinate care for those beneficiaries residing in the county. Selective Provider Contracting: The Waiver would give counties more authority to select their provider network. Counties, however, cannot discriminate against providers, must ensure an adequate provider network, and must guarantee beneficiary access to all covered services. Provider Appeals Process: The Waiver provides a process whereby providers can appeal to the county if they are not selected to contract with the county. Providers can also appeal to the State on the basis of ensuring network adequacy. Provider Certification: The State will partner with counties to certify DMC providers, with counties conducting application and on-site reviews and issuing provisional certification, and the State issuing final approval. • • • • Clear State and County Roles: Counties will be responsible for oversight and monitoring of providers as specified in their DMC contract with the State. Coordination: The Waiver supports coordination across systems, such as requiring counties to enter into MOUs with Medi-Cal managed care health plans for referrals and coordination, and requiring county SUD services to collaborate with criminal justice partners. Authorization and Utilization Management: The Waiver provides that counties will authorize services and ensure utilization management. Workforce: The Waiver will expand the pool of Medi-Cal eligible service providers to include licensed practitioners of the healing arts (LPHAs) for the assessment of beneficiaries, and other services within their scope of practice. • • Program Improvement: The Waiver promotes patient-centered, evidence-based practices, including medication-assisted treatment services, and increasing system capacity for youth services. Voluntary County Opt-In Demonstration: The proposed Waiver will be operational in counties that elect to opt into this organized DMC delivery system and agree to meet the specified requirements. Opt-in counties could choose to create an organized delivery system separate from Medi-Cal managed care, or could contract with Medi-Cal managed care plans to provide the DMC benefits. In a county that does not opt-in, there will be no change in DMC services from the current delivery system. * Potential Relief from IMD Exclusion: As an element of the Waiver proposal, DHCS is requesting the CMS approve an exception to the IMD payment exclusion for residential treatment services in those counties that opt-in to this demonstration. If CMS approval is granted, federal funds would be available to provide short-term residential treatment services to all eligible adults in facilities over 16 beds, and inpatient voluntary detox in chemical dependency treatment facilities and freestanding psychiatric facilities over 16 beds. The former process required counties to certify their total DMC expenses through the CPE process. DHCS then drew down FFP based on that total expense. Counties could then pay their contracted providers less than the total certified expense and retain the difference to cover county administrative expenses. CMS has stated that DHCS can only reimburse counties with the DMC reimbursement rate for the CPE-certified total direct service expense, and must reimburse counties for county administrative costs through a separate process. Therefore, effective July 1, 2014, DHCS has begun reimbursing counties for administrative DMC expenses through a separate invoicing process. For DMC claims with service dates on or after July 1, 2014, counties shall claim reimbursement for administrative DMC expenses separately from direct service expenses. • Such administrative expenses must be expenses actually incurred, and cannot be estimated expenses. • County administrative expenses will be limited to 15% of the DMC-reimbursable part of the county’s direct service expenses. What are county administrative DMC expenses? County administrative DMC expenses are expenses actually incurred as the result of providing county-operated DMC services, or as the result of administrative activities by a county as part of its business relationship with contracted providers, to provide DMC services. What are direct service expenses? Direct service expenses are those which have a clear, direct, and documented relationship to services that are provided to beneficiaries, i.e. • Compensation of employees for time devoted and identified specifically with the delivery of a DMC service; • Cost of materials spent specifically on the delivery of a DMC service. • Cost of maintaining facilities used to deliver DMC services. • Depreciation or lease costs of buildings and equipment used to deliver DMC services; and • Cost of services provided by contract. What are indirect service expenses? Indirect service expenses are those that are incurred for a common or joint purpose which benefits more than one cost objective, and are not readily assignable to the cost objectives specifically benefited. Since such indirect expenses benefit the provision of DMC services, or administration of DMC services, a portion of such expenses may be allocated to county administrative costs. Typical indirect expenses include: • Compensation of county employees for time not devoted specifically to the delivery of a reimbursable activity, or performance of specific administrative activity; • Allocated, indirect non-personnel expenses such as rent, utilities, insurance, and depreciation of county facilities; • Allocated, indirect personnel expenses to cover management services such as Director’s Office, Human Resources, Accounting, Budgeting, I.T., Business Services, Legal, etc. The initial Information Notice from DHCS (14-033) did not include provisions for counties to claim for quality assurance, utilization review, and Medi-Cal compliance oversight activities, all of which counties are required to do under the new DMC contracts. However, DHCS has indicated that a new Information Notice is being prepared that will stipulate how counties may claim reimbursement for these activities as administrative expenses.