Abnormal movements in children
Abnormal movements in children
Dr E Lubbe
Prof I Smuts
Dept Paediatrics
PAH
Bibliography
• Paediatrics and Child Health
Goovadia and
Wittenberg
• Rudolph`s Fundamentals of
Paediatrics
Rudolph et all
• Movement Disorders in
Children
Fernandez-Alverez and
Aicardi
Control of Movement
Cerebellum
•Control of movement patterns
•Motor learning
•Judge speed, force and direction
•Coordinator of information
•Receives information from
•Muscle spindles
•Labyrinth, eyes, parietal cortex
•Joints
•Pressure receptors
+
Extra pyramidal system
•Basal ganglia
•Thalamus
•Subthalamic nuclei
•Substantia nigra
•Red nucleus
•Brainstem reticular formation
Fluent movement
Start and stop of movement
Functional equilibrium in EPS
Ach
Dopamine
• Tics
• Tremors
• Chorea
• Dystonias
• Stereotypies
• Myoclonus
• Ataxia
Overview
Involuntary movements
• Abnormalities in structural and biochemical function of the nuclear masses of the basal ganglia
• Not under voluntary control
• Patient usually can’t stop them
• Without apparent purpose
• Aggravated by physical, emotional and mental stress
Differentiating between types
SLOW
Abn movement
FAST
Dystonias
Athetosis
Rhythmic
Tremor
Stereotyped
(involuntary)
Non-stereotyped
Not
Rhythmic
Tics
Myoclonus
Chorea
Tics
(complex stereotyped movement)
• Most common movement disorder in children
• Motor: eye blinking, shoulder shrug..
Vocal: squeaking, cough, sniffing…
Sensory: sensation ‘clothes not right’..
• Can be supressed ; relief when expressed again
• Lessens in sleep
• Aggravated by stress / anxiety
DSM IV
• Tics many times a day nearly every day
• Significant impairment or marked distress
• Onset < 18 yr
• Not due to drug or illness
Transient Chronic Tourette’s
Single/multiple motor AND/OR vocal
Single/multiple motor OR vocal
Multiple motor
AND single/multiple vocal
=/ > 4 weeks
< 1 year
> 1 year
Not tic free >
3 months
> 1 year
Not tic free >
3 months
• Tourettes Syndrome:
- combination motor and vocal tics
- present > 1 year
- onset before 18 years
not only present during use of psychotropic drugs
• Vocal tics can include echolalia, palilalia and coprolalia but rarer than led to believe in lay press
(present in about 20%)
• One third of cases asymptomatic by 17 years
Diagnosis
• Clinical
• Clues:
– Previous “normal” phenomena (throat clearing, eye blinking)
– Family history tics / OCD
– Features ADHD
– Urge
– Awareness occurrence
– ABILITY TO SUPPRESS
– No functional disability
– Can persist in sleep
• Diff dx:
• Chorea
• Myoclonus
• Stereotypies
• Compulsions
• Pseudotics
• Secondary – ass Strep infection “PANDAS”
Associated disorders
• Obsessions and compulsions - OCD
• ADHD
50 – 60% of TS precedes tics by 2-3 years
• Sleep disorders
• Learning problems 5X more special ed
• Behavioural problems
• Mood disorders
Tics
TS
OCD
ADHD
• Genetics: lot of data pointing to inheritable disorder
– probably autosomal dominant with variable expression
• Treatment:
-Pharmacological treatment only indicated if tics become incapacitating – rarely needed
Haloperidol usually effective
-Management of co-morbid disorders probably more important!
-
Associated with Strep inf:
PANDAS
• “Paediatric Autoimmune Neuropsychiatric
Disorder associated with Streptococcal infection”
• Tics , dystonia = broader spectrum movement disorders post GABHS infections
• Emotional and behavioural changes common – OCD, anxiety, “personality change”, social phobias…
• Auto-antibody @basal ganglia
• Criteria diagnosis:
1. Prepubertal
2. Tics or OCD
3. Sudden onset / fluctuating course
4. Ass with GABHS inf.
5. Neurological abn.
• ? Re role antibiotics / immune modulation / subgroup Tourette’s
Differentiating between types
SLOW
Abn movement
FAST
Dystonias
Athetosis
Rhythmic
Tremor
Stereotyped
(involuntary)
Non-stereotyped
Not
Rhythmic
Tics
Myoclonus
Chorea
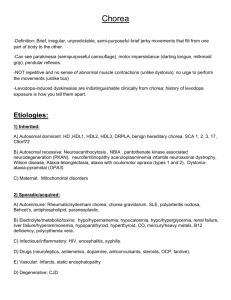
Chorea
(involuntary, arythmical, asymmetric, sudden, brief, >proximal)
150 causes described!
• Infectious:
– Rheumatic fever / Sydenham chorea
– Herpes encephalitis
– HIV
• Systemic diseases:
– SLE
• Metabolic:
– Wilson`s disease
– Galactosaemia
• Vascular:
– Cyanotic heart disease
• Intoxication:
– CO
– Methyl alcohol
• Primary genetic:
– Benign hereditary
– Huntington`s (presents in children with hypokinesia )
Sydenham Chorea
• Described in 1686
• Major feature of Rheumatic Fever
• In older than 10 year group: > in girls
• Later symptom
• Progressive – starts with behaviour problems, clumsiness, difficulty writing , restlessness then after weeks chorea becomes evident
• Present weeks to months; usually good outcome
Clinical manoevres:
• “Milk maid sign” : let child grasp index finger of examiner
• Ask child to extend arms above head with palms upward – will find it difficult to maintain the pose and will excacerbate chorea.
Differentiating between types
SLOW
Abn movement
FAST
Dystonias
Athetosis
Rhythmic
Tremor
Stereotyped
(involuntary)
Non-stereotyped
Not
Rhythmic
Tics
Myoclonus
Chorea
Dystonia
(co-contraction; abn. posture)
• Def: involuntary sustained or intermittent muscle contractions causing twisting or repetitive movements, abnormal postures or both. Can affect any part of the body incl. arms, legs, trunk, neck, eyelids, face, vocal cords. Can be painful
• Disappears with sleep
• Caused by an imbalance of neurotransmitters
Classification
• Primary:
– Idiopathic torsion dystonia
– Transient idiopathic dystonia of infants
– Juvenile parkinsonism
• Secondary:
– Metabolic diseases
– Drug induced
– Stroke, trauma, tumour, neurodegenerative
• In children two major types
– Primary torsion dystonia
– Dopa-responsive dystonia
• Genetic in origin – most autosomal dominant with variable penetration. Begins in feet and spreads to become generalised
• Severely disabling; cognition spared
• Watch out – these can look bizarre. Do not mistake for a psychogenic disorder; rather refer.
Dyskinetic CP
• 2 groups : Choreoathetotic and dystonic
• Often severe hypoxia in term baby; previously kernicterus
• History of insult + UMN signs
• Incidence of MR 30%
Athetosis
• Alternating dystonia
• Tone alternates between flexion and extension
• Distal muscles more affected than proximal
• Slow writhing movements
Stereotypies
• Voluntary often rhythmical movements – e.g. head banging, head rolling, thumb sucking. Selfstimulating behaviour can also be included here.
• Can occur in otherwise normal children
- head banging: 5% - 15 % normal infants (9 mo to 3yrs; >boys)
• Some patterns more prevalent in children with mental retardation and behaviour disorders like autism – e.g. self- mutilation, bruxism, hand washing.
Differentiating between types
SLOW
Abn movement
FAST
Dystonias
Athetosis
Rhythmic
Tremor
Stereotyped
(involuntary)
Non-stereotyped
Not
Rhythmic
Tics
Myoclonus
Chorea
Tremors
(rapid rhythmical)
• Worsened by activity and anti-gravity posture; classified as rest, postural & kinetic
• Cerebellar: typical intention tremor
• Non-cerebellar:
– Idiopathic:
• Chronic – physiological; essential (familial)
• Transient – jitteriness; shuddering attacks
– Secondary:
• Malnutrition – vit B12 defficiency ; Kwashiorkor
• Hydrocephalus
Myoclonus
(simple, sudden, single)
• Physiological:
– Sleep myoclonus
– Startle responses (awake)
• Non-epileptic:
– Benign neonatal sleep myoclonus
– Benign myoclonus of early infancy
• Epileptic:
– Myoclonic epilepsy
– Component of epileptic syndromes with different seizure types
Cerebellar Disorders
Cerebellar signs
1. Ataxia
2. Hypotonia
3. Dysarthria / abn speech
4. Dysmetria: Struggle to judge distance
5. Dysdiadochokinesia: Struggle to start and stop rapid movements
6. Nystagmus
Ataxia - 3 broad categories
• Acute ataxia
• Chronic non-progressive
• Chronic progressive
Acute ataxia
• Sudden onset
• Can’t walk
• Extremely clumsy
• Can’t feed due to tremor
• Dysarthria
• Nystagmus unusual
• Look for signs of infections e.g. chickenpox
• History of possible intoxication
• If signs are symmetrical, no raised ICP, and no focal signs, usually benign
Acute ataxia: Aetiology
• Infections
– Cerebellar abscess
– Viral cerebellitis
– Bacterial
• Metabolic:
– Organic acidurias
– Leigh’s encephalopaties
– Hypoglycaemia
– Hyperammonaemia
• Toxins
– Alcohol
– Phenytoin
– Phenobarbitone,
– Lead
– Glue
– Vit A
• Posterior fossa tumour
• Vascular
– Haemorrhage
– Embolism
– AVM
• Pseudo-ataxia
Chronic non progressive ataxia
• Ataxic/Hypotonic CP
• Often a congenital malformation of the cerebellum
Aetiology: Chronic Non progressive ataxia
– Perinatal insults
• Birth asphyxia
• Metabolic
• Intra ventricular haemorrhage
• Meningitis
– Congenital malformations
• Primary cerebellar hypoplasia
• Hydrocephalus
– Foetal alcohol syndrome
– Joubert syndrome
– Cerebellar/ kidney associations
– Postnatal acquired
• Hypoxia
• Hypoglycaemia
• Chronic phenytoin
• Thiamine deficiency
• Trauma
Chronic progressive ataxia
• Lesion in cerebellum with loss of:
– Purkinje cells
– Cerebellar nuclei
– Afferent or efferent pathways
• Olivary atrophy
• Spinocerebellar degeneration
• Post column demyelination
• Peripheral nerve lesion
Ataxia telangiectasia
• Progressive ataxia(1-4 years)
• Abnormal eye movements - oculomotor apraxia
• Telangiectasia(3years-adolescence)
• Cutaneous manifestations
• High risk for malignancies
• Abnormality in cellular and humoral immunity
• Elevated alpha feto protein
Ataxia-Telangiectasia
• Slowly progressive cerebellar ataxia
• Telangiectasis of skin and congunctivae
• Frequent sinobronchopulmonary infections
• Chorea-athetosis
• Malignancies – lymphoreticular
• Sensitivity to ionizing radiation
• Ocularmotor apraxia
Ataxia-Telangiectasia
• Most common cause for progressive ataxia in children under 10 next to posterior fossa tumours!
Chronic progressive
• Friedreich’s ataxia
– Onset before 20 years
– Autosomal recessive inheritance
– Progressive ataxia - gait difficulties, speech problems
– No nystagmus
– Weakness
– Positive Babinski but absent ankle and knee reflexes - involvement of the corticospinal tract
– Loss of position and vibration sense
– Positive Romberg test - involvement of the posterior columns
– Bladder dysfunction
– Involvement of cranial nerves
– Scoliosis
– Cardiomyopathy
– Diabetes mellitis