Metabolic Diseases
advertisement
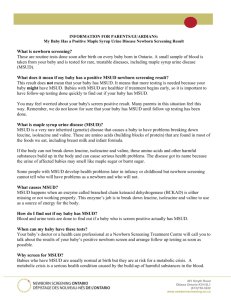
Management of Metabolic Disease Kathryn Camp, MS, RD, CSP Metabolic disease is all about Food and Nutrition Case Study--JC 11.5 mo male with MSUD presents to metabolic clinic for continued mgt of his IEM. PMHx: FT, normal at birth. Poor feeding and increased lethargy 1st week of life. Frequent calls to MD--mother told this was normal behavior DOL 7 to 10--continued poor feeding and lethargy; was taken to the pediatrician and placed on Prosobee formula DOL 11--unarousable. Admitted to hospital for dehydration and begun on nasogastric tube feeds of Similac. Admit labs: WBC 12.0, UA 1+ ketones, CO2 19, anion gap 8, glucose 63. Sepsis workup begun Cont: Neurological status began to deteriorate and by DOL 19 he was given the presumptive diagnosis of MSUD based on his course and the sweet smell noted in his urine. Several hours after the dx was given, he had respiratory arrest, was placed on the ventilator, and peritoneal dialysis was begun. Initial serum amino acid levels (umol/L): leucine 6,200(47-155) valine 677 (64-294) isoleucine 392 (31-86) Cont: G- tube and Nissen placed at 4 wks of age and he was begun on metabolic formula. He has had several hospitalizations since that time with reported difficulties with reflux, gagging, intolerance to feeds, and seizure activity. Normal growth. Diagnosed with static encephalopathy. Maple Syrup Urine Disease Autosomal recessive inheritance Infants are normal at birth In severe forms, seizures, apnea, and death can occur within 10 days of birth Branched-chain -ketoacid dehydrogenase complex (BCKAD) deficiency Elevated levels of branched-chain ketoacids, their amino acid precursors, and alloisoleucine Treatment These children decompensate within the first few days of life – Delayed or missed dx leads to coma and death Goal is to identify affected infants before they crash – Not all states screen for MSUD – Screen is often not back before the child becomes symptomatic Treatment cont: Diagnose and initiate treatment as soon as possible – Emergency therapy – Life-time dietary treatment – Liver transplantation – Gene therapy and others are still some years in the future Dietary Protein Catabolized Tissue Protein Leucine Isoleucine Valine -ketoisocaproic -keto-3-methylvaleric -ketoisoval acetyl-CoA + Acetoacetate acetyl-CoA + Propionyl-CoA Succinyl-CoA branched-chain -ketoacid dehydrogenase complex Propionyl-CoA Succinyl-CoA NCA Metabolic Patient Population Glutaric Acidemia type 1 – 22 mo old dx at 6.5 mo after 1 mo of irritability, seizures, and dystonic movements. You may see her some time over the winter. Methylmalonic acidemia – 5 yr old was a frequent flyer; now in better control Tyrosinemia type 2 – 1 college student PKU – 10 mo old – A set of 2 yr old identical twins, former 25 wk premmies – 2 high school students Homocystinemia – 1 high school student MCAD – 12 mo old dx on NBS Our population changes constantly and you never know what you might get! – Good possibility that one or more of these kids will be admitted to the ER or the Ward on YOUR watch Overview Newborn Screening Dietary treatment Emergency management Long term issues Newborn Screening Definition Newborn screening in the US is a public health program aimed at the early identification of conditions for which early and timely intervention can prevent or reduce associated mortality and morbidity – Adapted from the “Newborn Screening Task Force Report”, Pediatrics 106:383-427, 2000. Child with PKU – born before NBS Full expression of this genetic disease + gene mutation + environmental exposure + genetics - exposure - genetics + genetics + exposure Brief History of NBS Began in 1963 in MA with screening for PKU – Guthrie developed a bacterial inhibition assay for phenylalanine using a dried blood filter paper card. By 1967, mandatory PKU testing in most states 70’s and 80’s, additional tests from the “Guthrie” card were developed (galactosemia, MSUD, biotinidase, homocystinemia, congenital hypothyroidism, CAH) – Up to 8 diseases were included in NBS (varied by state) 1990’s, tandum mass spectrometry technology was developed which allows for detection of a greater number of disorders of amino acid, organic acid, and fatty acid metabolism (see handout) Newborn Screening is State Public Health Activity Federal govt recommends screening for PKU, congenital hypothyroidism, and sickle cell disease Each state is responsible for designing and implementing its own program – Which disorders to include in the screen – Whether parental consent is required 33 states allow exemptions for religious reasons 13 states allow exemptions for any reason – Whether they will use a state-run lab or contract out to a private lab Just because TMS technology is used in a state, it does not mean that that state performs the “expanded” screen. Criteria for Newborn Screening Program The Disorder – Clearly defined (known) – Treatable, with trt initiated in the neonatal period – Reasonable incidence The Screening Test – Rapid turnaround time – High sensitivity and specificity – Reasonable cost Follow-up – Locate babies with + screens – Provide appropriate referral to CONFIRM diagnosis and provide treatment Relevance to YOU Don’t assume that a reportedly “normal” NBS on a sick baby rules out the possibility of a metabolic disease Further, the New York state NBS program has reported through genetic identification that the blood sample for 1 out of 800 babies screened was incorrectly labeled http://genes-r-us.uthscsa.edu Why Does Dietary Treatment Keep these Kids Alive and Protect Their Brains? Because…... Biochemical defect is known – absent or minimal production of enzyme system that breaks down dietary constituents With the amino acidopathies (MSUD, MMA, PKU), defect involves dietary constituents that are “essential” – Restrict the precursors to the toxic metabolites We can use consequences of the defect to design our therapy What Happens in PKU? Food Phenylalanine Catabolized tissue Absent phenylalanine hydroxylase tyrosine DOPA, NE, EPI, Melanin Increased PHE and Production of Alternate Products Phenylalanine Phenylpyruvate Phenyllactate Phenylacetate tyrosine Product of Blocked Reaction Is Not Made Phenylalanine Phenylpyruvate Phenyllactate Phenylacetate tyrosine DOPA, NE, EPI, Melanin Solution: Phenylalanine tyrosine Supply Product Four Therapeutic Strategies to Treat Amino Acidopathies 1. Enhance Anabolism and Depress Catabolism Provide sufficient energy and protein to prevent catabolism of body muscle and release of free amino acids – high energy feedings – medical formulas devoid of the offending amino acids – low protein products Prevent fasting 2. Restrict Toxic Substrate MSUD: leucine, isoleucine, and valine MMA: isoleucine, methionine, threonine, valine, odd-chained FA, gut origin short-chained fats Note: the amino acids are essential and sufficient amounts must be provided to support normal growth 3. Supplement Conditionally Essential Nutrients MSUD, MMA, GA, MCAD – Carnitine helps excrete organic acids in the urine PKU – Tyrosine Homocystinemia – cystine 4. Replace Deficient Cofactors MSUD: Thiamin – pharmacologic doses – 100 to 500 mg oral/day – USRDA is 1 mg/day MMA: Vitamin B12 – 1 mg po or IM GA: Riboflavin – 200 mg/d Goals of Dietary Treatment Correct biochemical abnormalities Support normal growth and development Maintain normal nutritional status Minimize physical manifestations – MSUD:urine free of branched-chain ketoacids – MMA: urine free of abn organic acids Designing a Diet for a Person with MSUD, PKU, MMA, GA Titrated amount of essential amino acids are provided by “whole” protein Remaining protein needed for body growth and maintenance is supplied by “medical formula” – purified amino acid based products – also contain CHO, fat, vitamins, and minerals Extra calories come from “free” foods Presentation and Illness are Life Threatening Situations! Acute Mgt ABC’s Hydrate—promote renal excretion of offending metabolites Treat biochemical derangements – Bicarb for acidosis—IV drip – IV Glucose (D12 peripherally, more if central) – Carnitine—MMA 100-150 mg/kg; MSUD 50 mg/kg Withhold whole protein (max 24-48 hrs) to prevent further buildup of toxic metabolites Acute Mgt, cont Remove toxic metabolites – Hydration – Dialysis (only at presentation in a comatose patient with MMA) Prevent catabolism – Dextrose (>10%) – Insulin if needed Prevent constipation and promote gut motility for MMA Prevent increased ICP in MSUD—use zofran for nausea Initiate Nutrition Support Immediately! High energy feeds – 120-150 kcal/kg infants – 80-100 kcal/kg children If the gut works, use it PO, n/g, g-tube – metabolic formula without added whole protein (initially restrict offending amino acids) Notify endocrine service Acute Mgt, cont: If gut cannot be used or if sufficient formula cannot be delivered enterally: IV via central line peripheral line hypertonic dextrose 12% dex lipids lipids – replace electrolytes incl 4-6 mEq sodium Can use a combination, e.g: – drip feeds of formula to supply non-offending amino acids + IV dex Monitoring During Acute Mgt MSUD and MMA Serum amino acids daily – whole blood (green top) to Children’s (M-F) – Pediatrix filter paper card (available in endo clinic conference room file cabinet) if 3-4 day turnaround OK MSUD – Add purified ILE and VAL to metabolic formula when blood levels reach upper limit of normal; add LEU as whole protein when levels reach upper limits of normal. MMA – Add VAL as whole protein when levels reach upper limits of normal. Long-Term Dietary Management Using published guidelines, clinical picture, and biochemical parameters, establish the dietary prescription Establish the Dietary Rx Newly dx 1 month old with MSUD Per kg LEU: 60-100 mg ILE: 36-60 mg VAL: 42-70 mg Protein: 3-3.5 g Kcal: 120 Fluid: 125-150 ml Components of the Medical Formula Four ingredients: 1. Infant formula provides LEU, ILE, VAL 2. Ketonex-1 provides remaining protein 3. Polycose provides any needed calories 4. Water Additional ILE and VAL – solution of 10 mg purified amino acids/ml prepared by pharmacy or parents (if they have an appropriate scale) Metabolic Formulas Life After Exclusive Formula Feeding Solid foods are added to the infant’s diet in an age appropriate manner Begin with cereals and advance to vegetables then fruit Amounts are calculated using exchange lists and food composition tables Every bite of food must be weighed! Infant/child/adult continues to drink medical formula Foods in the Diet of a Person with PKU, MSUD, MMA NO meat, poultry, fish, dairy, legumes Limited grains, vegetables, fruit Unlimited pure carbohydrates or fat Limited in MMA dietary protein catabolized muscle Phenylalanine Restrict precursor tyrosine Supply Product 8 year old with PKU—Reg Foods Breakfast: Lunch 65 Snack: Dinner: 14 Snack: mg Phe Kcal 1 slice white bread 101 67 8 oz medical formula 0 200 1 rice cake w 1 t marg 40 70 1/2 cup noodle soup 103 89 5 saltine crackers 1.4 68 8 oz medical formula 2 c popcorn w 4 t marg 4 oz apple juice 120 g pasta 3 T tomato sauce 0 91 2 745 0.6 200 190 107 445 13 8 oz medical formula Fruit ice 1/2 oz potato chips 0 10 44 200 124 76 Diet Rx: Phe: 345 mg Pro: 52 g Kcal: 2000 3.5 x PHE Rx Typical Day’s Intake—LP Foods Breakfast: Lunch 65 Snack: Dinner: 14 Snack: mg Phe Kcal 1 slice low pro bread 11 104 8 oz medical formula 0 200 1 rice cake w 1 t marg 40 70 1/2 cup low pro soup 48 67 5 saltine crackers 1.4 68 8 oz medical formula 2 c popcorn w 4 t marg 4 oz apple juice 120 g low protein pasta 3 T tomato sauce 0 91 2 12 0.6 200 190 107 432 13 Diet Rx: Phe: 345 mg Pro: 52 g Kcal: 2000 Reality Check 1 oz cheese 355 mg 8 oz medical formula Fruit ice 1/2 oz potato chips 0 10 44 200 124 76 1 oz chicken 345 mg Cost Comparison of LP Products and Their Regular Counterparts Food Item Regular Low Protein Flour, 16 oz $0.27 $5.00 Spaghetti, 16 oz $1.25 $10.00 Crackers, 16 oz $0.79 $15.00 Rice, 16 oz $0.55 $10.00 Cream Cheese, 8 oz $1.99 $5.60 Am Cheese, 10 oz $2.30 $10.00 Tomato Sauce, 4 oz $0.25 $4.00 Shipping and handling runs $5.00 to $25.00 per order Practical Issues of Dietary Treatment Compliance – these diets are complicated!! – harder to adhere to as the child ages Cost – $$$$ medical formula and low protein foods – insurance coverage Repeated blood draws and doctor’s visits New Therapies Liver transplantation in MSUD and MMA Gene Therapy MSUD Symposium 2000 Danvers, MA Happy Halloween !!