A CASE OF MALIGNANT HYPERTENSION
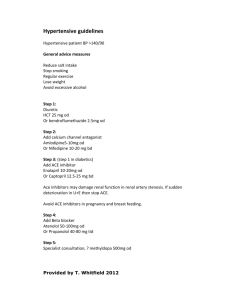
advertisement
A CASE OF MALIGNANT HYPERTENSION DR ANN HOLMES GPST2 CASE Px, 56, c/o loss of central vision R eye, blurred vision L +mild generalised headache. ∆hypertension 5yrs ago but had stopped taking tablets entirely 12/12 ago due to £ issues. Previously on 3 meds but can’t recall names. Feels well otherwise. PMH unremarkable. Smokes 5/day; <14U ETOH GP refers: BP 200/130, ?papilloedema Ophthalmoscopy: frank papilloedemaGd IV hypertensive retinopathy ECG: LVH Urine dipstix: protein++++, trace blood Hb13; ur9,creat240,eGFR14 glucose N LFTs N, neuro exam NAD Mild leg pitting oedema Moved to HDU, arterial line, catheterised, labetolol+GTN infusions Further investigations: cortisol, TFTs, nephritic screen, myeloma screen, urine alb:creat ratio, urgent renal USS+CT head, renin-angiotensinogen levels, urine 24hr metanephrine+catecholamines, lipid profile Renal, endocrine+ophthalmology teams informed Renal artery angiography HDU for 6/7 whilst BP slowly reduced. Antihypertensives recommenced with omission of ACE inhibitors. ∆ Malignant hypertension secondary to severe renal artery stenosis: R 100% occlusion; L 80% Candidate for possible revascularization How common is it? In 1964, Holley et al data from 295 autopsies performed in their institution during a 10month period. The mean age at death was 61 years. The prevalence rate of renal artery stenosis was 27% of 256 cases identified as having history of hypertension, while 56% showed significant stenosis (>50% luminal narrowing), and, among normotensive patients, 17% had severe renal artery stenosis (>80% luminal narrowing). Among those older than 70 years, 62% had severe renal artery stenosis. Similar results with other studies. Causes of Renovascular hypoperfusion Atheroma>90% Takayasu’s arteritis>60% in Indian subcontinent+Far East Fibromuscualar hyperplasia Rarely:PAN,AVM,neurofibramatosis NB Renal artery stenosis prevalence cauc:black 2:1 Numerous referrals with high BP >180 systolic and headache… Definition of malignant hypertension? Severe hypertension with WITH papilloedema + end organ damage Primary care: Urine dipstix key ?proteinuria+/-blood; ophthalmoscopy. ECG NOT diagnosed on numbers alone <1% hypertensives develop: rare Cause: Essential hypertension in 80% Blacks, 2-30% Caucasians; renal disease the rest High BPloss of autoregulation; endothelial injury, vascular smooth muscle hypertrophy+collagen depositionluminal narrowing with ischaemia+infarction of end organs Concurrent pressure triggered natriuresis+SNS stimulationfurther BP Mortality 90% at 1yr if untreated NICE hypertension 2011 Severe hypertension (syst>180 or diastol>110) at diagnosis: Same day referral if accelerated hypertension with papilloedema/retinal haems + BP>180/110 or suspect phaeochromocytoma Otherwise assess for end organ damage, don’t wait for ambulatory BP/serial BD home recordings+consider starting treatment with A/C +review A/C if <55 +C+D;stepwise addition of therapy Review 1/52ly or sooner post med change for progress aiming for <140/90 if <80 (<150/90 if >80; 130/80 if DM Then further diuretic/low dose spironolactone dep on K/-blocker if not tolerated Monitor U+Es within 1/12 Refer if not controlled on 4 meds Check compliance Px education-address lifestyle issues CVD risk factor assess+manage references http://www.patient.co.uk/doctor/Ren al-Vascular-Disease.htm http://emedicine.medscape.com/artic le/245023-overview Clinical opthalmology 3rd edn:Kanski p369 NICE guidelines 2011 hypertension