Septic miscarriage
Miscarriage
Dr Mariem Gweder
DHR MSc MRCOG DOGUS
Definition
Miscarriage = Spontaneous abortion
Spontaneous loss of a fetus before the
24th week of pregnancy.
WHO definition: loss of an embryo or fetus weighing 500 grams or less, (20 to
22 weeks or less.
(Pregnancy losses after the 20th week are called preterm deliveries.)
Incidence
Occurs in about 15% to 20% of all clinical pregnancies,
60% to 70% occur during the first trimester.
Most miscarriages occur during the first 7 weeks of pregnancy.
The rate of miscarriage drops after the detection of fetal heart.
Classifications
Clinical / ultrasonic
Threatened Miscarriage : bleeding seen, cervix closed, the fetus is viable.
Inevitable Miscarriage : the cervix has already dilated, but the fetus has yet to be expelled. This usually will progress to a complete miscarriage.
Complete Miscarriage: is when all products of conception have been expelled. Endometrium is less than 15mm thick on
US.
Incomplete Miscarriage: part of conception is passed, cervical os is open, and the retained part is more than 15mm thick
Delayed or missed miscarriage: the embryo or fetus has died, but the os is closed.
Anembryonic pregnancy (blighted ovum) An empty gestational sac, the embryo is either absent or stopped growing
Complications
Septic miscarriage: missed or incomplete miscarrige becomes infected.
Recurrent pregnancy loss: three consecutive miscarriages.
Causes & Risk factors
First trimester
Chromosomal abnormalities: majority of cases
-Advanced maternal age: more likely to occur in older women highest after 40
-Woman suffering RPL,
-H/O birth defects.
Causes & Risk factors
??Progesterone deficiency may be another cause.
No study has shown that first-trimester progesterone supplements reduce the risk
Polycystic ovary syndrome.: metformin significantly lowers the rate but insufficient evidence of safety,
Maternal disease: Hypothyroidism, autoimmune diseases, APL, uncontrolled diabetes
Infections,: TORCH, acute febrile illness, pylonephritis.
Smoking, Recreation drugs, Alcohol, Antidepressants
Physical trauma, exposure to environmental toxins,
Multiple pregnancy
Causes
Second trimester (PTL)
Uterine malformation: Up to 15%
Uterine fibroids
Cervical problems (cervical incompetence)
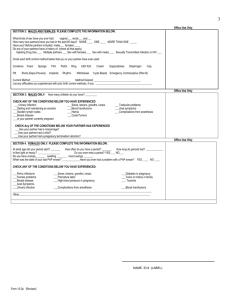
Diagnosis
Symptoms
Examination
Ultrasound: confirmation
BHCG
Microscopically
Genetic for abnormal chromosomes
Symptoms
The most common symptom is vaginal bleeding with or without abdominal cramps
Up to 30% of women will have first trimester bleeding or spotting
Low back pain or abdominal pain (dull, sharp, or cramping)
Tissue or clot-like material that passes from the vagina
Examination
General examination: vital signs
Abdominal examination : fundal level
Pelvic exam, cervical dilatation or effacement, blood clot, POC in the cervical os
Abdominal / vaginal ultrasound : gestational age, fetal heart, retained products.
Investigations
Blood type (if Rh-negative, anti-D immune globulin is needed.
Complete blood count (CBC): HB to determine blood loss, WBC and differential to rule out infection
HCG to confirm pregnancy
HCG (quantitative) to rule out ectopic pregnancy
HVS and Blood C/S if septic
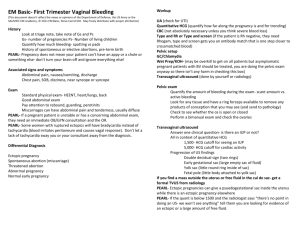
Management
B
C
If in shock or heavy bleeding act as emergency:
A
No treatment
-Threatened : bed rest has no proven benefit.
-Complete
Only
Counsel
Anti-D if needed
Follow up:(weekly)
Management options
For
- Incomplete abortion,
- Anembryonic (empty sac)
-Missed abortion
“Early Pregnancy Assessment Unit”
Options:
Expectant (Conservative)
Medical or
Surgical
Expectant (conservative)
No treatment
“wait & see”
(65–80%) will pass naturally within two to six weeks.
avoids the side effects and complications of medications and surgery risk of mild bleeding, need for unplanned surgical treatment, and incomplete miscarriage
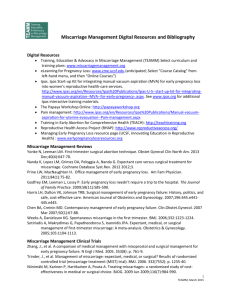
Medical management
-
-
Mifepristone (anti-progesterone) oral, followed by (36-
48h)
Misoprostol: vaginal or oral tabs: repeat in 4-6 hrs if required
Success rate 95% will complete within a few days.
Indications:
Patient choice
Second trimester: Surgical evacuation is unsafe
First trimester : >10 weeks, before D&C & cervix is closed
(Misoprostol 400 mcg to ripen the cervix 3-4 hrs prior to dilatation)
Contraindication to surgery or anaesthesia ,DIC
Advantages:
Fewer risks and complications
Less cost
Greater patient satisfaction
Surgical treatment
Vacuum aspiration or Traditional (D&C or E&C)
Fast
Less bleeding,
Less pain
Convenient for karyotype analysis (cytogenetic or molecular),
The patient is febrile (>37.5
0 C)
◦ After appropriate antimicrobial management
The patient or your health facilities are incapable of appropriate follow up
Complications :
injury to the cervix (e.g. cervical incompetence) perforation of the uterus,
Asherman's syndrome: scarring of the endometrium
Septic miscarriage
Occurs when the tissue from a missed or incomplete miscarrige becomes infected.
Unsafe abortion: gram negative, E.Coli Streptococci Staphylococci
Bacteroides Chlostridium Perfringens
STIs: Niesseria Gonorrhea Chlamydia Trochomatis
Presentation:
Prolonged or heavy vaginal bleedin offensive vaginal discharge
Fever hypotension
Hypothermia, oliguria
Septic shock may lead to kidney failure and disseminated intravascular coagulation(DIC). chronic pain, PID, and infertility
Risk of septicaemia and maternal death.
Septic miscarriage management
Intravenous fluids
Broad-spectrum IV antibiotics should be given until the fever is gone.
D&C or misoprostol
Recurrent pregnancy loss
(RPL)
Recurrent miscarriage (habitual abortion) three consecutive miscarriages.
1% of miscarriages
Causes
Chromosomal: balanced translocation or Robertsonian translocation in one of parents
Endocrinal
Thrombophilia, Antiphospholipid syndrome
Anatomical: cong anomalies, fibroids
Cervical incompetence
Work up
Ultrasound: 2D, 3D, Sonohysterography
Hysterosalpingogram (HSG)
Hysteroscopy
Karyotyping
Women with unexplained recurrent miscarriage have an excellent prognosis for
Future pregnancy
After miscarriage
The tissue passed should be sent to histopathology to exclude molar pregnancy.
Possible to become pregnant immediately.
However, it is recommended that women wait one normal menstrual cycle before trying to become pregnant again.
Anti-D for RH negative.
Counseling, support , explanation
Follow up
Summary
Miscarriage mostly occurs in first trimester
Majority of cases are due to chromosomal abnormalities
Classification is clinical and ultrasonic
Proper counseling is needed
Patient choice should be considered in management options.