BMI PowerPoint Presentation 48x36
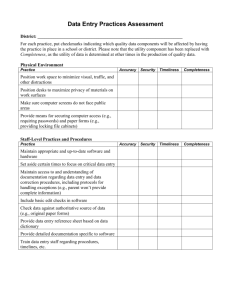
advertisement
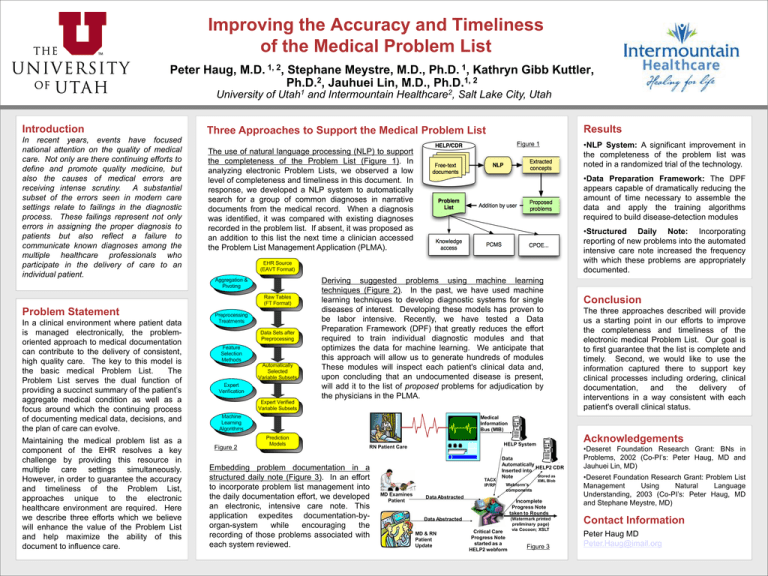
Improving the Accuracy and Timeliness of the Medical Problem List Peter Haug, 1, 2 M.D. , University of Introduction In recent years, events have focused national attention on the quality of medical care. Not only are there continuing efforts to define and promote quality medicine, but also the causes of medical errors are receiving intense scrutiny. A substantial subset of the errors seen in modern care settings relate to failings in the diagnostic process. These failings represent not only errors in assigning the proper diagnosis to patients but also reflect a failure to communicate known diagnoses among the multiple healthcare professionals who participate in the delivery of care to an individual patient. Stephane Meystre, M.D., Kathryn Gibb Kuttler, 2 1, 2 Ph.D. , Jauhuei Lin, M.D., Ph.D. 1 Utah and Intermountain 2 Healthcare , Salt Lake City, Utah Results Three Approaches to Support the Medical Problem List Figure 1 The use of natural language processing (NLP) to support the completeness of the Problem List (Figure 1). In analyzing electronic Problem Lists, we observed a low level of completeness and timeliness in this document. In response, we developed a NLP system to automatically search for a group of common diagnoses in narrative documents from the medical record. When a diagnosis was identified, it was compared with existing diagnoses recorded in the problem list. If absent, it was proposed as an addition to this list the next time a clinician accessed the Problem List Management Application (PLMA). In a clinical environment where patient data is managed electronically, the problemoriented approach to medical documentation can contribute to the delivery of consistent, high quality care. The key to this model is the basic medical Problem List. The Problem List serves the dual function of providing a succinct summary of the patient’s aggregate medical condition as well as a focus around which the continuing process of documenting medical data, decisions, and the plan of care can evolve. •NLP System: A significant improvement in the completeness of the problem list was noted in a randomized trial of the technology. •Data Preparation Framework: The DPF appears capable of dramatically reducing the amount of time necessary to assemble the data and apply the training algorithms required to build disease-detection modules •Structured Daily Note: Incorporating reporting of new problems into the automated intensive care note increased the frequency with which these problems are appropriately documented. Deriving suggested problems using machine learning techniques (Figure 2). In the past, we have used machine learning techniques to develop diagnostic systems for single diseases of interest. Developing these models has proven to be labor intensive. Recently, we have tested a Data Preparation Framework (DPF) that greatly reduces the effort required to train individual diagnostic modules and that optimizes the data for machine learning. We anticipate that this approach will allow us to generate hundreds of modules These modules will inspect each patient's clinical data and, upon concluding that an undocumented disease is present, will add it to the list of proposed problems for adjudication by the physicians in the PLMA. Problem Statement Maintaining the medical problem list as a component of the EHR resolves a key challenge by providing this resource in multiple care settings simultaneously. However, in order to guarantee the accuracy and timeliness of the Problem List, approaches unique to the electronic healthcare environment are required. Here we describe three efforts which we believe will enhance the value of the Problem List and help maximize the ability of this document to influence care. 1 Ph.D. , Conclusion The three approaches described will provide us a starting point in our efforts to improve the completeness and timeliness of the electronic medical Problem List. Our goal is to first guarantee that the list is complete and timely. Second, we would like to use the information captured there to support key clinical processes including ordering, clinical documentation, and the delivery of interventions in a way consistent with each patient's overall clinical status. Medical Information Bus (MIB) Figure 2 HELP System RN Patient Care Embedding problem documentation in a structured daily note (Figure 3). In an effort to incorporate problem list management into the daily documentation effort, we developed an electronic, intensive care note. This application expedites documentation-byorgan-system while encouraging the recording of those problems associated with each system reviewed. TACX IP/RP MD Examines Patient Acknowledgements Data Automatically HELP2 CDR Inserted into Stored as Note Webform’s components Data Abstracted Incomplete Progress Note taken to Rounds Data Abstracted MD & RN Patient Update XML Blob Critical Care Progress Note started as a HELP2 webform (Watermark printed preliminary page) via Cocoon; XSLT Figure 3 •Deseret Foundation Research Grant: BNs in Problems, 2002 (Co-PI’s: Peter Haug, MD and Jauhuei Lin, MD) •Deseret Foundation Research Grant: Problem List Management Using Natural Language Understanding, 2003 (Co-PI’s: Peter Haug, MD and Stephane Meystre, MD) Contact Information Peter Haug MD Peter.Haug@imail.org