Developing the Nurse Practitioner Role in Community Palliative Care
advertisement

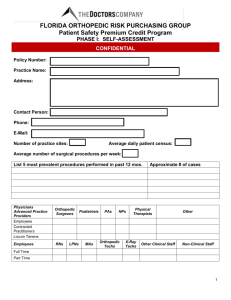
Developing the Nurse Practitioner Role in Community Palliative Care Leanne Davey Nurse Practitioner, Palliative Care Royal District Nursing Service Northern Region Collaborative Project • Royal District Nursing Service & • Melbourne CityMission Palliative Care Service • Development of Clinical Practice Guidelines (CPG’s) & Medication Formulary Implementing the NP role in the Community setting • Appointment of Project Manager • Key areas of work undertaken: – Gaining an in-depth understanding of the Drugs, Poisons and Controlled Substances Regulations 2006 (Vic) in order to identify areas to be addressed – Writing a Policy and Procedure to support the NP prescribing & authorising rights – Developing a Position Description – Identifying equipment needed for the role – Developing a specific set of codes – Developing a comprehensive Communication Strategy Policy and Procedure-Nurse Practitioner role in medication and diagnostic tests Policy and Procedure was derived from the Drugs, Poisons and Controlled Substances Regulations 2006 (Vic) and includes: • Definitions of terms used in the policy • General policy statement • Processes in relation to: – – – – – Prescribing medicines Seeking consent to the NP prescribing Disclosure of drug use Oral instructions in an emergency Schedule 8 permit and notification requirements Policy and Procedure-Nurse Practitioner role in medication and diagnostic tests (cont’d) – Confirming prescriptions – Authorising medicines – Disposing of unused schedule 8 medicine ampoules – Transporting client medicines – Authorising diagnostic investigations – Communicating with doctors or hospital Policy and Procedure-Nurse Practitioner role in medication and diagnostic tests (cont’d) – Referring to community based service/inpatient for admission – Giving advice to a Doctor – Giving notification of a drug dependent person – Giving notification of fraudulent obtaining of drugs and poisons – Process where GP writes script and NP writes authorisation in the home Position Description • Job purpose • Key Position functions - Clinical Practice - Quality Management - Research and Continuous Improvement - Collaboration and Partnership Approach - Professional Development • Skills/knowledge/attributes • Qualifications Equipment to support NP role • Private prescription pad • Electronic access to copy of: – Therapeutic Guidelines – MIMS online, and – Australian Medicines Handbook • Nurse Practitioner stamp • Prompt card Activity Codes • Activity codes developed to reflect practice • Codes exclusive to NP role • Data terms and definitions for codes developed to reflect and capture the extended practices • Supporting evidence for the NP role Communication with internal & external Stakeholders Communication strategy included: • Developing letters to introduce the role • Arranging visits to Pharmacies and GP’s • Writing articles for newsletters • Developing a road show presentation • Producing Business cards Issues to address • Carrying of drugs by NP • Inability to access PBS • Expense of private scripts Strategies to address the challenge • Decision not to carry drugs • Costing of medications on private script • Forging relationships with Pharmacies, the Pharmacy Board and Guild • Development of private prescription pad • Authorising medications in collaboration with the GP or specialist Demonstrating Continuing Competency • • • • Professional portfolio Development of new activity codes Clinical Supervision Review/update CPG’s every 2-3 years Conclusion • Sharing of information/experience • Consult/contact • Process for using RDNS forms & documentation -Written request to Sharon McNeil, RDNS Policy Officer -Need to acknowledge RDNS on form/documentation