Glucose Monitoring
advertisement
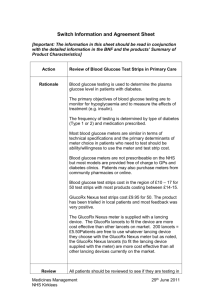
Glucose Monitoring Ceri Jones 2014 Glucose Monitoring Why? Who? Benefits of Glucose Monitoring Improve glycaemic control? Empowerment Hypoglycaemia? Intercurrent illness/sick day rules Pre-pregnancy, pregnancy Driving Special clinical situations Intensive regimens Glucose monitoring Studies ROSSO SMBG decreased diabetes-related morbidity and allcause mortality SMBG may be associated with a healthier lifestyle and/or better disease management Faas SMBG in T2DM patients questionable needs good RCT Coster SMBG established in clinical practice optimal use not established. Evidence suggests may not be essential for all Reasons for not BGM Cost The NHS spends approximately £90 million on blood glucose testing materials. This is 40% more than on oral hypoglycaemic agents (£64 million). Inaccuracies Out of date strips Contaminated strips Incorrect meter calibration Meter reading incorrectly Sticky fingers Incorrect sample size Temperature of equipment Rhondda Cynon Taff 12 months Costs 2003-2004 Hazard Warning A Department of Health hazard warning notice (HN (Hazard)(87), stated that all staff should be trained in the use of Blood Glucose meters including the Quality Assurance process by appropriate trained staff. Diabetes UK advise that no member of staff, registered or otherwise should:- perform blood glucose monitoring unless they have a sound knowledge base of diabetes. have received training on blood glucose monitoring using the meter specific to their place of employment. be aware of how to interpret the reading(s) obtained and the subsequent action to be taken. POCT Cwm Taf Health Board’s “Point of Care Testing Policy” (2010), define Point of Care testing as:- “Analytical tests undertaken by non-laboratory staff outside a recognised diagnostics laboratory” The policy also states:- “Only staff whose training and competence has been established and documented should use any Point of Care Testing device.” Case Study 1 A person with Diabetes on a complex regimen of treatments was admitted to a hospital intensive care unit . A blood glucose was measured using a blood glucose meter, a high result indicated hyperglycaemia and insulin treatment was initiated. A separate sample sent to the hospital laboratory gave a markedly different result. A thorough investigation, revealed that the glucose meter should not be used on patients who were on treatments containing maltose. The patient suffered significant hypoglycaemia and complications because staff were unaware of this limitation. Key points • Users should be aware of the manufacturer’s instructions and contra-indications for use. • Such information should be incorporated into training of all staff using such a device. • In this case, the device itself was not faulty, but was used contrary to the manufacturer’s recommendations. • The MHRA does not seek to apportion blame but instead to advise others on how to avoid similar problems. Case Study 2 Outbreaks of hepatitis B were reported from several environments where blood glucose monitoring was being carried out for multiple patients. Thorough investigations identified that care workers were found to be using lancing devices intended for self-use (by one patient only) to take blood samples from multiple patients. This use of the wrong sort of lancing device was implicated in the transmission of the virus. Key points • Be aware that employing the wrong sort of lancing device can cause cross infection. • Use a disposable single-use lancing device where the entire device is thrown away after use, or employ a reusable lancing device that is intended, by the manufacturer, for taking samples from more than one patient. • Users should review current practice to ensure that appropriate devices are provided and used BGM Guidelines NSF Standards 3 and 4 All children, young people and adults with diabetes will receive a service which encourages partnership in decision-making, supports them in managing their diabetes and helps them to adopt and maintain a healthy lifestyle. All adults with diabetes will receive high-quality care throughout their lifetime, including support to optimise the control of their blood glucose. All children and young people with diabetes will receive consistently high-quality care and they, with their families and others involved in their day-to-day care, will be supported to optimise the control of their blood glucose. BGM Guidelines NICE Guidelines, 2002 Self-monitoring should not be considered as a stand alone intervention. Self-monitoring should be taught if the need/purpose is clear and agreed with the patient. Self-monitoring can be used in conjunction with appropriate therapy as part of integrated self-care. BGM Guidelines DUK Position Statement People with diabetes should have access to home blood glucose monitoring based on individual clinical need, informed consent and not on ability to pay. The majority of diabetes care is provided by the individual. It is essential that people with diabetes be provided with the education and tools in order to be able to manage their diabetes for themselves. Glucose Monitoring Technology and technique Technology Meters numbers available Not on prescription Coding & quality control Lancing Devices Professional Individual patient Single use Not on prescription Lancets Available on prescription Quality Assurance Training Quality Control Accuracy of equipment Reliability of results Quality Control solutions Meter Strips Quality Control - when? New meter New test strips Change of Batteries Test strips left open Meter dropped/damaged Unexpected result Failed Quality Control Check expiry dates Were tests carried out in correct order Repeat levels 1 and 2 again Change QC solution & Repeat Change test strips (change code) Lancing Systems Multiple use device with single use lancet – patients Single use lancet - professional Sharps Sharps box should be used Sharps must NOT be put in rubbish Advice if no sharps box Sharps disposal service tel: 01443 494700 Glucose Monitoring Frequency of testing and when? Diet & Metformin If stable patients should be taught the principles of HBGM and if appropriate should monitor once a week fasting Sulphonylureas If stable patients should be taught the principles of HBGM and encouraged to monitor twice a week fasting plus at 1 other time Once daily or BD Insulin If stable patients should be taught the principles of HBGM and encouraged to monitor twice a day 2-3 times per week. Basal Bolus Insulin Regimen If stable they should be encouraged to monitor 4 times a day 2-3 times per week. Factors affecting BG levels Food Exercise Physical activity Illness and pain Medication OHAs Insulin Alcohol Emotional stress When to test more frequently? Medication is changed Insulin started Sick day rules / illness Risk of hypoglycaemia Exercise Advised by DSN or P/N Driving Pregnant/planning a family Monitoring Errors Out of date strips Contaminated strips Incorrect meter coding Incorrect meter Hands not clean Temperature of equipment Contraindications Severe dehydration Hypotension / Shock / Peripheral Circulatory failure Hyperosmolar non-ketotic Coma (HONK) Diabetic Ketoacidosis (DKA) Venous sample to lab Home Blood Glucose Monitoring If stable people controlled on diet alone or diet and Metformin and/or Glitazones and/or Acarbose should be taught the principles of HBGM and if appropriate should monitor once a week fasting If stable people controlled with Insulin secretagogues and diet should be taught the principles of HBGM and encouraged to monitor twice a week fasting plus at 1 other time If stable people controlled with BD or OD insulin should be taught the principles of HBGM and encouraged to monitor twice a day 23 times per week. If stable people controlled with basal bolus insulin should be taught the principles of HBGM and encouraged to monitor 4 times a day 2-3 times per week. Test strips and lancets should not be issued on a repeat prescription. They should be requested from the practice nurse six monthly or yearly HbA1c is an excellent indicator of long-term control. Test more frequently if Continuing education Monitoring Frequency Quality assurance Coding Acting on results HbA1c Medication is changed Insulin started Sick day rules / illness Risk of hypoglycaemia Exercise Advised by DSN or P/N Driving Pregnant/planning a family Patients should not buy their own meters, these will be provided free of charge via the practice nurse. Practices to keep a stock of meters (arranged via the diabetes facilitators) for PWD DAFNE CSII There should be no blanket ban on Home Blood Glucose Monitoring (HBGM) Individual needs change, some may need to test more frequently than others. HbA1c is an excellent indicator of long-term control